STEMI
Author Credentials
Author: Navdeep Sekhon, MD / Baylor College of Medicine
Editor: Moises Gallegos, MD, MPH / Stanford University School of Medicine
Update: 2023
Case Study
A 55 year old female stumbles into triage diaphoretic and clutching her chest. She states, “I don’t feel good, and my chest really hurts. Can you help me?”
The triage nurse quickly places the patient in a wheelchair and rushes the patient into Critical Care Room 1. The patient’s vital signs are: T 98.6F, Pulse 30 beats per minute, blood pressure is 80/40 mmHg with an Oxygen saturation of 92% on a nasal cannula.
The nurse quickly obtains the following ECG and tells you, “Doc, the patient in room one is pretty sick. Do you mind coming over and checking her out?”

Figure 1. ECG of the 55 year old. Courtesy of Navdeep Sekhon, MD. Used with permission.
As you look at the ECG and walk into the room, you begin to plan your next steps.
Objectives
By the end of this module, the student will be able to:
Define a STEMI
Give a differential diagnosis of ST elevations (it’s not always a STEMI)
Recognize the varied clinical presentations of patients with STEMI
Understand regional blood vessel distribution correlation on ECG
Introduction
“Time is Muscle” -Ancient Cardiology Proverb
ST-elevation myocardial infarctions (STEMIs) are one of the classic emergencies in Emergency Medicine. Rapid recognition and treatment are essential to ensure that patients have optimal outcomes.
The phrase “time is muscle” is apt when talking about a STEMI because every minute of delay in treatment increases the amount of myocardial death. In addition, multiple studies show that reduction in door-to-intervention time decreases mortality and morbidity. It is because of the importance of early recognition and treatment of STEMIs that patients who present to the Emergency Department with chest pain should have an electrocardiogram done within 10 minutes of presentation to the Emergency Department. Overall, the quicker a patient undergoes revascularization, the better outcome they will have.
What is a STEMI?
Acute coronary syndrome (ACS) is a spectrum of disease characterized by limitations in the amount of blood perfusing the heart and resulting in ischemia. This spectrum of disease includes:
Unstable Angina
NSTEMI
STEMI
STEMI is the most severe type of acute coronary syndrome and, untreated, has the worst mortality and morbidity. STEMIs are recognized by their characteristic ECG findings of having ST-elevations and are associated with complete or near-complete occlusion of a coronary artery. The etiology of most STEMIs are the rupture of an atherosclerotic plaque which subsequently occludes a coronary artery causing transmural myocardial infarction. Less common causes of STEMIs include:
Coronary artery dissection: which is more common in young adults
Coronary artery vasospasm: which can occur with the use of sympathomimetic drugs (cocaine, methamphetamine).
A discussion of the ECG criteria for a STEMI is discussed in more detail in the section Diagnostic Testing in this online chapter.
Initial Actions and Primary Survey
The ABC’s
Airway: On initial evaluation, the patient’s airway should be assessed. If the patient’s airway is not intact, it should be secured.
Breathing: The patient's breathing and lung sounds should be assessed. Patients may require supplemental oxygen and even mechanical ventilation to oxygenate and ventilate appropriately.
Circulation: The patient’s pulses and blood pressure should be assessed. If the patient is hypotensive, fluids and/or inotropes may need to be initiated.
Initial Actions
The ABC’s should be assessed and stabilized on all patients
Rapid recognition of a STEMI is crucial to optimizing patient outcomes when it comes to morbidity and mortality. Thus, rapid performance and interpretation of an ECG are crucial for the patient with a STEMI.
Goal: First Medical Contact to ECG time is 10 minutes
Some Emergency Medical Services (EMS) will transmit ECGs to the hospital from the field to promote the rapid recognition and treatment of a STEMI.
A rapid history should be performed to ensure that there is no alternative diagnosis and to assess the patient's risk for STEMI. In particular:
A quick history regarding the presenting complaint should be performed
The patient should be asked questions regarding cardiac risk factors and prior history of cardiovascular disease/interventions
A physical examination should be performed to screen for other possible causes of chest pain and assess for cardiogenic shock.
Interventional Cardiology should be emergently consulted on the recognition of STEMI to provide emergent treatment.
A chest radiograph can be performed to screen for the other causes of chest pain. Special attention should be paid to look for:
a widened mediastinum which may be caused by aortic dissection. Aortic dissections have been known to cause STEMIs by the disruption of blood flow through the coronary artery.
evidence of volume overload.
Presentation
Clinical Presentation
STEMIs can present with a variety of different presentations, even without the patient endorsing chest pain. Thus, it is important to keep a broad differential when evaluating patients that present to the Emergency Department.
Patients who are experiencing an acute STEMI are classically described as presenting with chest pressure or crushing chest pain associated with shortness of breath, nausea/vomiting, or diaphoresis. The chest pain might be described as radiating into the patient’s neck, left arm, or jaw. Often times, they will appear visibly uncomfortable and may have a fist clutching the center of their chest. This classic finding of angina is known as the Levine’s sign.

Figure 2. Levine’s Sign. Picture courtesy of Navdeep Sekhon, MD.
It is important to remember, as noted in “The Approach to Chest Pain” module, that patients with a STEMI may not present with chest pain, but with other anginal equivalents like: nausea and vomiting, epigastric pain, fatigue, and/or shortness of breath. This may be more common in elderly, diabetic, and female patients. Thus, it is important to maintain a high index of suspicion for this emergent disease process.
Table 1. Signs and symptoms of a STEMI.
Diagnostic Testing
In patients who present with a possible STEMI, the following studies should be ordered:
ECG
Troponin
CBC
BMP
Chest radiograph (depending on the situation)
ECGs are the mainstay in diagnosing STEMIs, as there are characteristic ECG findings that help diagnose a STEMI. Physicians should not wait for a troponin level to return before activating the cath lab, as the diagnosis should be made on ECG alone and, as mentioned before, “time is muscle.”
Given the importance of rapid recognition of STEMIs to reduce patient’s mortality and morbidity, it is recommended that all patients with chest pain have a Door to ECG time of 10 minutes or less.
ECG Findings of a STEMI
The ECG Segments
Before we go into the ECG findings of a STEMI, it is important to identify the isoelectric line and the ST-segment on the ECG.
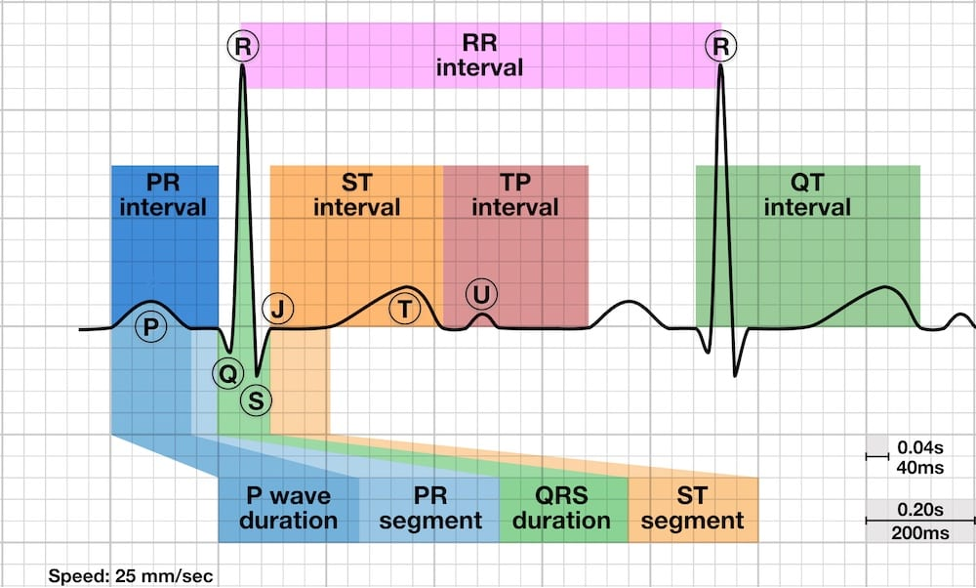
Figure 3. The segments of an ECG. Courtesy of Life in the Fast Lane and used via the https://creativecommons.org/licenses/by-nc-sa/4.0/. The original image is located at: PR segment • LITFL • ECG Library Basics.
The TP segment is the isoelectric line where there is no underlying cardiac electrical activity, and this is the baseline from which you measure all ST segment elevations or depressions. The TP segment is defined as the segment that starts at the end of the T wave and ends at the beginning of the P wave.
The ST segment is the portion of the ECG that starts at the end of the S wave and ends at the beginning of the T wave. Normally, it is isoelectric with the TP segment and represents the interval between ventricular depolarization and repolarization. Elevations or depressions of the ST segment can be a sign of myocardial ischemia and is important to recognize.
The J point is another part of the ECG that is important to know when trying to ascertain if an ECG shows a STEMI. The J point marks the change of inflection from the end of the S wave to the being of the ST segment (see Figure 4).

Figure 4. The J point and how to measure ST Segment elevation or depression. Original image courtesy of Life in the Fast Lane and used via the
https://creativecommons.org/licenses/by-nc-sa/4.0/
. The original image is located at:
PR segment • LITFL • ECG Library Basics
. Modified by Navdeep Sekhon, MD.
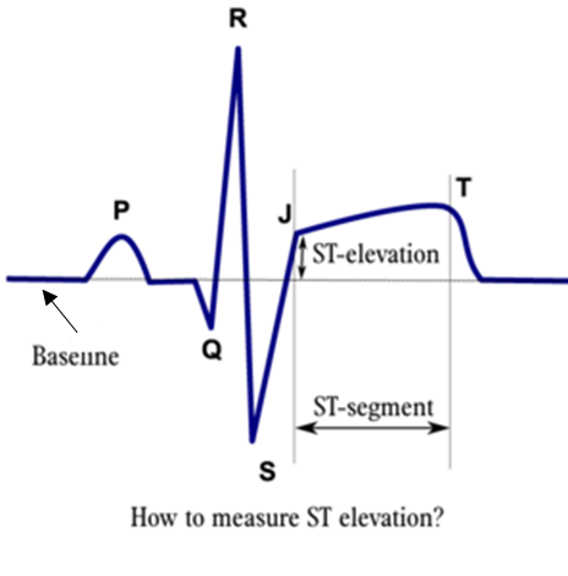
Figure 5. How to measure ST Segment elevation or depression. Original image courtesy of J.S.S.G de Jong, MD from the website ecgpedia.org. Used under the Creative Commons Attribution Non-commercial Share-alike License. https://creativecommons.org/licenses/by-nc-sa/3.0/. Website: ST Morphology - ECGpedia. Modified by Navdeep Sekhon, MD.
As Figures 4 and 5 demonstrate, the the degree of ST segment elevation is measured from the isoelectric line (the TP segment) to the J point, and is commonly measured in millimeters (1 small box=1mm)
Describing the ST Segment Morphology
The shape of the ST segment can be helpful in assessing whether an ECG demonstrates a STEMI. Classically the ST elevations are described as “tombstone” and convex in appearance. However, other morphologies such as concave or straight elevations might be seen in STEMI as well.
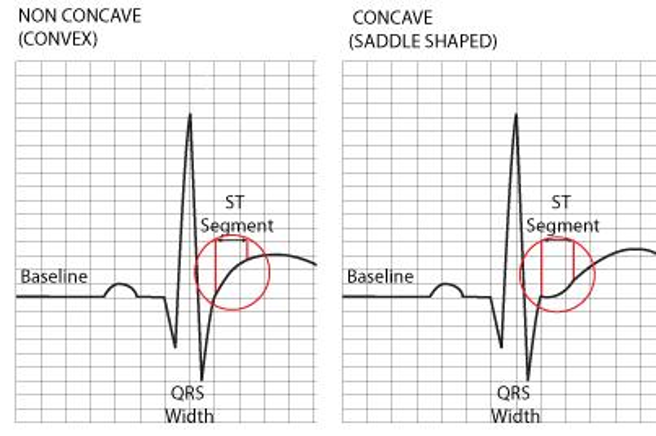
Figure 6. Concave vs Convex ST Segment. Courtesy of RCEM Learning. Used using the Creative Commons Attribution-NonCommercial 3.0 UK: England and Wales. https://creativecommons.org/licenses/by/3.0/. The original website is ST Elevation without Infarction - RCEMLearning.
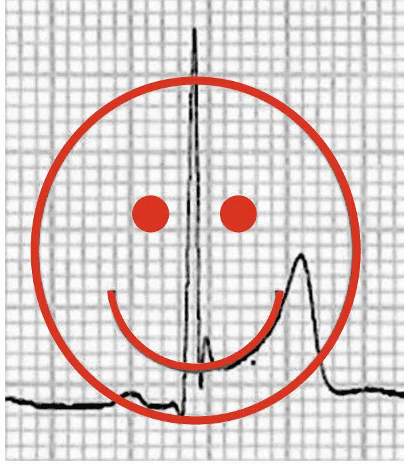
Figure 7. Concave ST segment was historically thought to be benign, but STEMIs can present with this morphology. Please review the whole ECG for signs of a STEMI, and do not only look at the morphology. Original image courtesy of Life in the Fast Lane and used via the https://creativecommons.org/licenses/by-nc-sa/4.0/. The original image is located at: Benign Early Repolarisation • LITFL • ECG Library Diagnosis.
The ECG Definition of a STEMI
Classically, STEMI is diagnosed if there is >1mm of ST elevation in two contiguous leads on the 12 lead ECG.
STEMI is defined by the European Society of Cardiology/ACCF/AHA/World Heart Federation Task Force for the Universal Definition of Myocardial Infarction as:
New ST Elevation at the J point in V2-3 of at least two contiguous leads
≥2mm in men
≥1.5mm in women
New ST Elevation in the J point of at least 1mm in two contiguous leads (except for V2-3)
An important point of caution is that these ECG definitions of STEMIs can miss acute coronary artery occlusion that may benefit from emergent reperfusion. It is sometimes helpful to think of the following saying when interpreting ECGs for a possible STEMI:
“Amateurs measure millimeters,
Professionals interpret the whole ECG.”
-Ancient Cardiology Proverb
Thus, it is important to interpret the whole ECG: the ST elevations, reciprocal changes, and the morphology of the ST segment WITH the clinical context. It is also important to note that the STEMI criteria above cannot be used with a Left Bundle Branch Block or a ventricular paced rhythm, where the Sgarbossa criteria can be applied instead.
Contiguous Leads
As you can see in the definitions listed above, it is important to understand what contiguous leads are in order to diagnose a STEMI. Simply speaking, contiguous leads are leads that represent arterial territories that are next to each other.
In general, contiguous leads are:
For the precordial leads, they are the neighboring leads (V3 and V4, for example)
II, III and AVF are contiguous leads for the inferior portion of the myocardium
I and AVL are contiguous leads for the high lateral portion of the heart (this one is often forgotten)
For the posterior leads, V7, V8 and V9 are contiguous leads
Evolution of ECG Changes in STEMI
The ECG in STEMI changes over time. This is important to note, as when the diagnosis is unclear, repeating ECGs can be helpful in making the diagnosis.
The general progression of the ECG changes in a STEMI follows:
Acute, hyperacute T waves form. These form in the first minutes to hours of a STEMI. A hyperacute T wave is characterized by an increase in the amplitude and the width of the T wave.
Next, ST elevations will develop.
Followed by the development of Q waves.
Later, the T wave will invert.
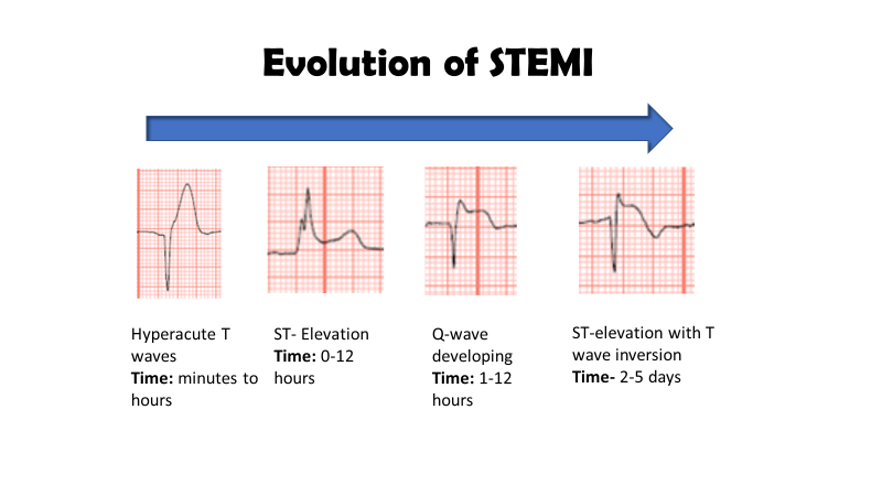
Figure 8. Evolution of ECG Changes in STEMI. Image courtesy of Navdeep Sekhon, MD.
Reciprocal Changes
Reciprocal changes in STEMIs are the ST depressions found on the ECG that are on the opposite side of the heart of the myocardial infarction. It is important to note that the absence of reciprocal changes does not preclude the presence of a STEMI, but the presence of reciprocal changes makes it more likely.
Table 2. Reciprocal changes in STEMI.
STEMI Territories
STEMIs are classically categorized by the portion of the heart that is affected by the myocardial infarction: anterior, posterior, lateral and inferior. By understanding which portion of the heart is affected, you also begin to determine which coronary artery is occluded. Please refer to the figure below for the territories.
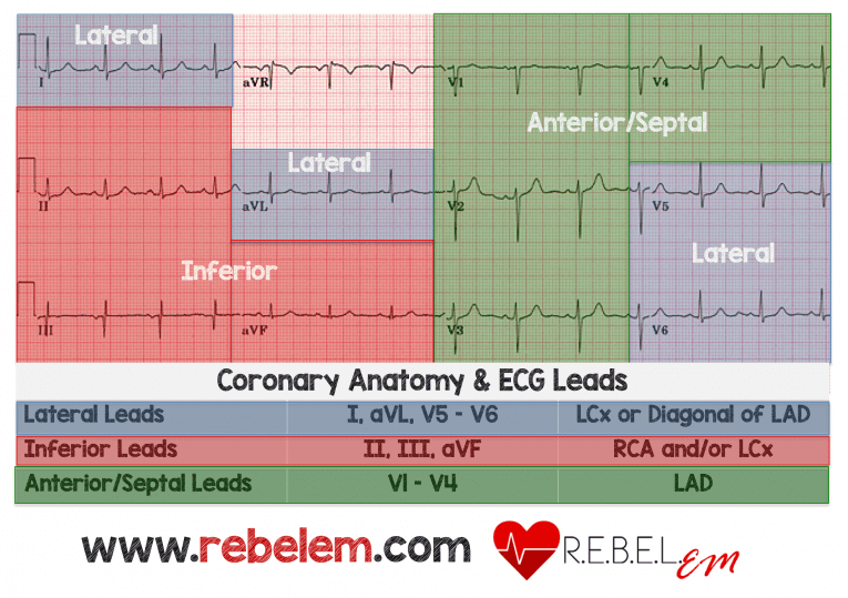 Figure 9. STEMI territories and vasculature. Courtesy of REBELEM and used under the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. Original image found on:
Rebellion in EM 2018: STEMI Equivalents by Tarlan Hedayati, MD - REBEL EM - Emergency Medicine Blog
Figure 9. STEMI territories and vasculature. Courtesy of REBELEM and used under the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. Original image found on:
Rebellion in EM 2018: STEMI Equivalents by Tarlan Hedayati, MD - REBEL EM - Emergency Medicine Blog
Table 3. STEMI territories and their vasculature.
Now, let’s discuss in more detail each kind of STEMI in more detail.
Anterior STEMI
Anterior STEMIs generally result from the occlusion of the left anterior descending coronary artery, and carries the worst prognosis of all STEMIs given the larger infarct size. Anterior STEMIs can be diagnosed by recognizing ST elevations in the anterior leads (V1-V4) and reciprocal changes in the inferior leads (II, III and AVF). An example of an anterior STEMI follows:
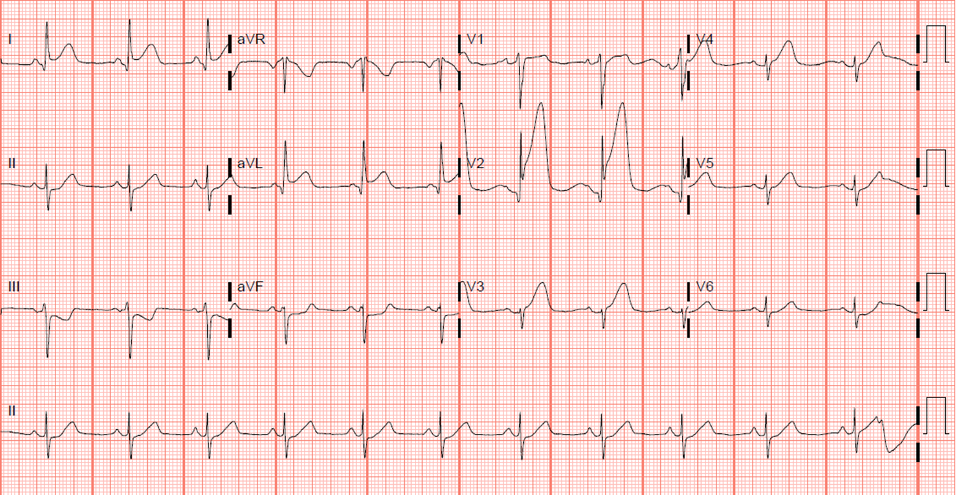
Figure 10. ECG of an anterior STEMI. The cardiac catheterization of this ECG demonstrated a 100% occlusion of the left anterior descending coronary artery. This ECG is courtesy of Navdeep Sekhon, MD.
Lateral STEMI
Lateral STEMIs generally result from the occlusion of the left circumflex coronary artery or the diagonal branch of the left anterior descending. On ECG, this is recognized by ST elevations in the lateral leads (V5-6) or the high lateral leads (I and AVL). It is important to remember that I and AVL are contiguous leads and ST elevations in these leads can signify a high-lateral STEMI. An example of a lateral STEMI follows.
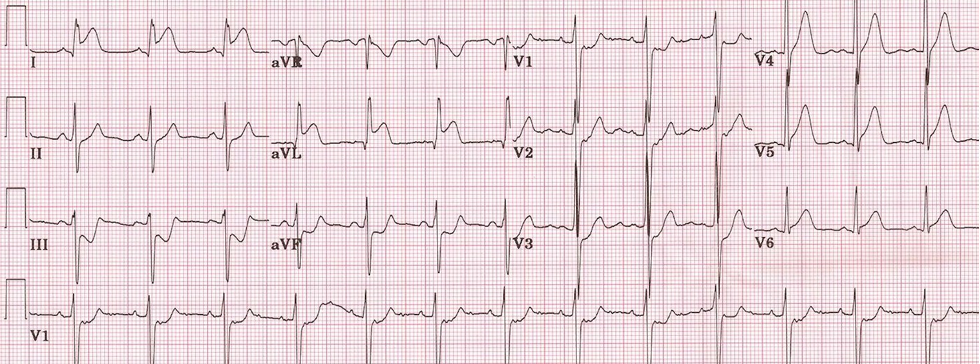
Figure 11. ECG of a lateral STEMI. Please note the ST elevations in I and AVL, which are the high lateral leads with reciprocal changes in III and AVF. ECG courtesy of Navdeep Sekhon, MD.
Inferior STEMI
In general, inferior STEMIs result from the occlusion of the Right Coronary Artery (70%) or the Left Circumflex. On ECG, this can be recognized with ST elevations in the inferior leads (II, III and AVF) with reciprocal changes in the high lateral leads (I and aVL). With these leads in particular, complete coronary occlusion can occur with less than 1mm in ST elevation in the anterior leads, so a high index of suspicion should be maintained. An example of an inferior STEMI is below.
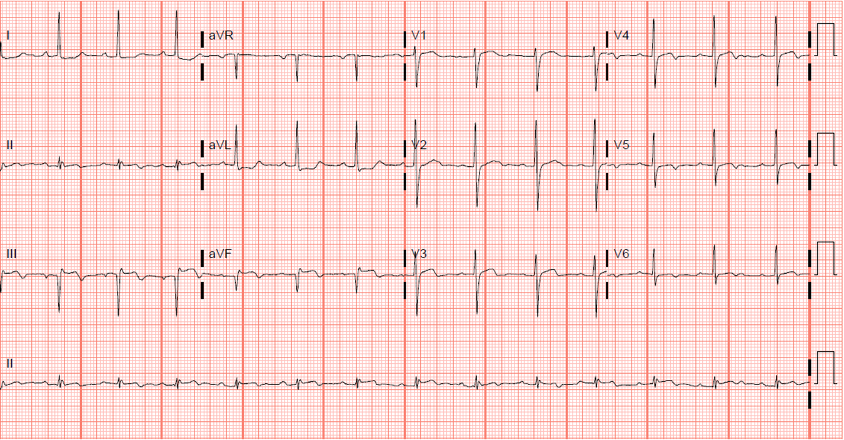
Figure 12. ECG of an inferior STEMI. Please note the ST elevations in leads II, III and AVF with the reciprocal ST depressions in leads I and AVL. The subsequent cardiac catheterization demonstrated a 100% occlusion of the right coronary artery. Image courtesy of Navdeep Sekhon, MD
A subset of inferior STEMIs are right ventricular infarcts, which are preload dependent. This is important to recognize because if they become hypotensive, fluids can be helpful. In addition, right ventricular infarcts should not be given nitroglycerin as it can precipitously drop their blood pressure.
A right ventricular infarct in the context of an inferior STEMI can be discovered by the following ECG findings:
The degree of ST-elevation on Lead III is greater than the degree of ST-elevation on Lead II
ST-elevation on Lead V4r on a right sided ECG (performed by flipping the precordial leads onto the right side of the chest)
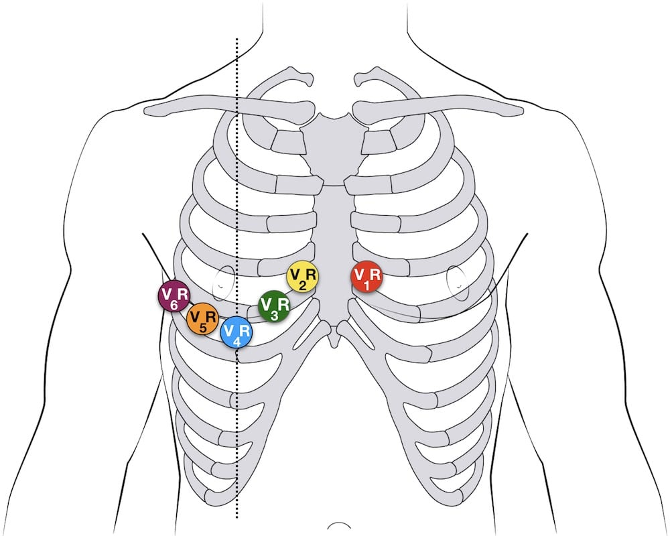
Figure 13. Lead placement for a right sided ECG. Image courtesy of Life in the Fast Lane and used under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Original image can be found at: Right Ventricular Infarction • LITFL • ECG Library Diagnosis.
Posterior STEMI
“Not all STEMIs have ST elevation”
-Old ECG proverb
When thinking of posterior STEMIs, it is important to remember the quote above, as these acute coronary artery occlusions can present without ST elevations on the 12 lead ECG. This occurs because the normal 12 lead ECG looks at the anterior part of the heart, and only the reciprocal changes of a posterior can be seen on the 12 lead ECG.
Posterior STEMIs are caused by an occlusion of posterior descending coronary artery. On a normal 12 lead ECG, it can be recognized by:
ST depression in the anterior leads
Prominent R waves in leads V2-3
Upright anterior T waves
An example of a posterior STEMI follows:

Figure 14. ECG of an posterior STEMI. Note the ST depressions in the anterior leads with the prominent R waves and the upright T waves. Image courtesy of Navdeep Sekhon, MD.
To help confirm your diagnosis, you can also perform a posterior ECG. This can be performed by placing the leads on the patient’s back. The leads should be placed:
V7- At the level of V6, place at the posterior axillary line
V8- At the tip of the scapula at the level of V6
V9- Left paraspinous region at the level of V6
To call a posterior STEMI, it is important to note that you only need 0.5mm of ST elevation in the posterior leads. An important thing to note is that the posterior ECG is not sensitive enough to rule out a posterior STEMI, so providers should act on the initial 12-lead ECG.
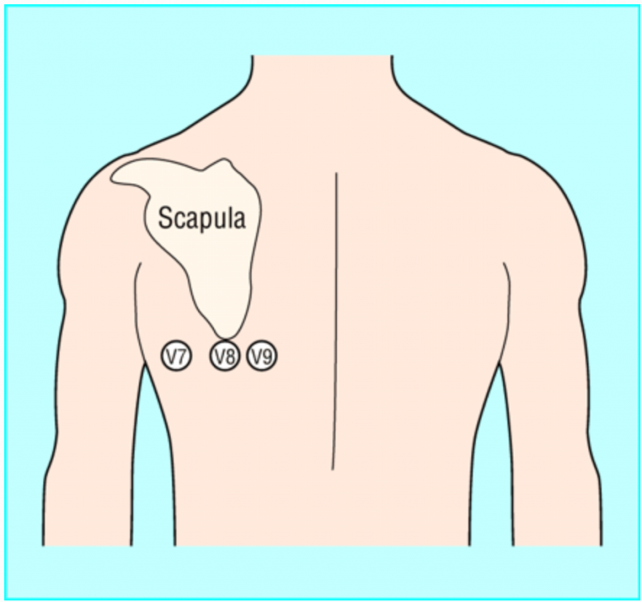
Figure 15. Lead placement for posterior ECG. Image courtesy of EMDocs under the Creative Commons Attribution 4.0 International License. emDOCs.net – Emergency Medicine EducationECG Pointers: Posterior MI - emDOCs.net - Emergency Medicine Education
STEMI Equivalents
De Winter’s Sign
The De Winter’s sign is a sign of an occlusion of the left anterior descending artery, and should be viewed as an equivalent to an anterior STEMI. The ECG findings of De Winter’s sign are:
Upsloping ST depression greater than 1mm in the precordial leads
Prominent, tall, and symmetrical T waves in the precoridal leads
Absence of ST elevation in the precordial leads
Reciprocal ST elevation of 0.5mm-1mm in AVR
An example of the ECG findings is shown below:
 Figure 16. De Winter’s sign. Please note the upsloping ST depression with the tall, symmetrical T Wave. Image courtesy of Life in the Fast Lane and used using the Creative
Commons Attribution-NonCommercial-ShareAlike 4.0 International Licence. https://creativecommons.org/licenses/by-nc-sa/4.0/.
Original image located on: De Winter T Wave • LITFL • ECG Library Diagnosis.
Figure 16. De Winter’s sign. Please note the upsloping ST depression with the tall, symmetrical T Wave. Image courtesy of Life in the Fast Lane and used using the Creative
Commons Attribution-NonCommercial-ShareAlike 4.0 International Licence. https://creativecommons.org/licenses/by-nc-sa/4.0/.
Original image located on: De Winter T Wave • LITFL • ECG Library Diagnosis.
Hyperacute T waves
Hyperacute T waves are the first ischemic changes in a STEMI. They are characterized by an increase in the height and width of the T wave. These large T waves tend to be asymmetrical. Early recognition of these hyperacute T waves is crucial to the management of the early STEMI.
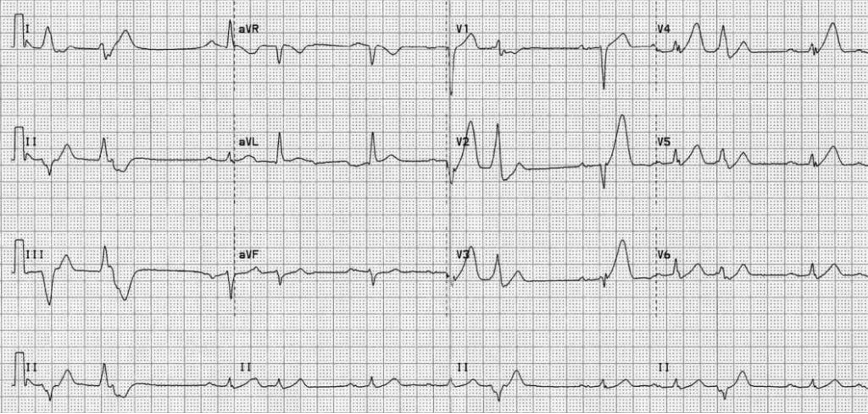 Figure 17. Hyperacute T wave of an early anterior STEMI. Please note the large, broad and asymmetrical T waves in the anterior leads. Courtesy of Life in the Fast Lane and used
under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The original image can be found on: ECG Case 009 • LITFL • ECG Top 100 Self-Assessment Quiz
Figure 17. Hyperacute T wave of an early anterior STEMI. Please note the large, broad and asymmetrical T waves in the anterior leads. Courtesy of Life in the Fast Lane and used
under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The original image can be found on: ECG Case 009 • LITFL • ECG Top 100 Self-Assessment Quiz
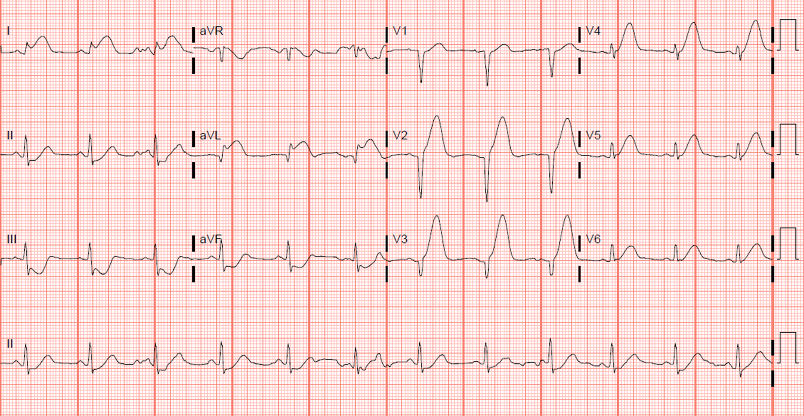 Figure 18. Hyperacute T waves of an anterior STEMI. Please note the large, broad and asymmetrical T waves in the anterior leads. This patient also has ST elevation in the high lateral
leads (I and AVL). The cardiac catheterization demonstrated a 100% lesion in the left anterior descending. Image courtesy of Navdeep Sekhon, MD.
Figure 18. Hyperacute T waves of an anterior STEMI. Please note the large, broad and asymmetrical T waves in the anterior leads. This patient also has ST elevation in the high lateral
leads (I and AVL). The cardiac catheterization demonstrated a 100% lesion in the left anterior descending. Image courtesy of Navdeep Sekhon, MD.
Left Bundle Branch Block with Sgarbossa Criteria
Historically, a new left bundle branch block (LBBB) was considered a STEMI equivalent. However, studies suggested that the true incidence of an acute coronary occlusion in a presumed new LBBB was low, and the American Heart Association dropped a new LBBB as a STEMI equivalent. It is important to note that some of these patients with a new LBBB will have an acute coronary occlusion. To make the patient with chest pain who has a LBBB even more challenging, the traditional STEMI criteria cannot be applied to an ECG with LBBB.
To overcome these hurdles, some providers will use a bedside echocardiogram to check for wall-motion abnormalities to try to identify patients with LBBB on ECG who have acute coronary artery occlusion.
The Sgarbossa criteria was developed to identify patients with LBBB or have a ventricular-paced rhythm who have a STEMI based on ECG findings. Before we discuss the Sgarbossa criteria, it is important to define concordant and discordant ST changes. Simply, concordant ST segment changes mean that the QRS segment amplitude and the ST segment deviation both point in the same direction. For example, concordant ST segment changes include:
ST segment elevation with a positive QRS amplitude
ST segment depression with a negative QRS amplitude
Conversely, discordant ST changes are changes when the amplitude of the QRS segment is opposite to the deviation of the ST segment. For example, discordant ST segment changes include:
ST segment elevation with a negative QRS amplitude
ST segment depression with a positive QRS amplitude.
 Figure 19. Concordant ST deviations. Note that the amplitude of the QRS segment and the ST deviation are in the same direction. Image courtesy of Navdeep Sekhon, MD.
Figure 19. Concordant ST deviations. Note that the amplitude of the QRS segment and the ST deviation are in the same direction. Image courtesy of Navdeep Sekhon, MD.
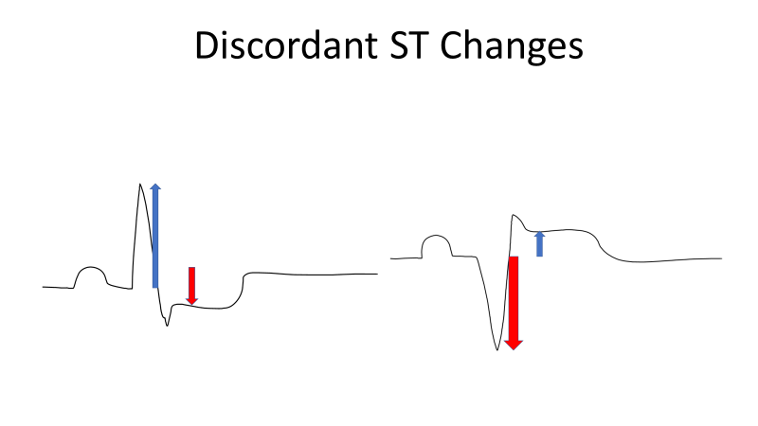 Figure 20. Discordant ST deviations. Note that the amplitude of the QRS amplitude and the ST segment are in the opposite directions. Image courtesy of Navdeep Sekhon, MD.
Figure 20. Discordant ST deviations. Note that the amplitude of the QRS amplitude and the ST segment are in the opposite directions. Image courtesy of Navdeep Sekhon, MD.
The Sgarbossa Criteria for STEMI in the context of LBBB or a ventricular paced rhythm are:
Concordant ST elevation > 1mm in leads with a positive QRS (score 5)
Discordant ST elevation > 1mm in leads V1-V3 (score 3)
Excessively discordant ST elevations > 5mm (score 2)
An ECG with a score greater than or equal to 3 is suggestive of a STEMI.
Differential diagnosis of ST elevations
The most serious cause of ST elevations on ECG is a ST segment elevation myocardial infarction (STEMI), however there are other possible etiologies. As usual, always consider the “worst first.” In borderline or atypical cases remember that timely diagnosis of STEMI is imperative to improve patient outcomes.
Pathologic ST-segment elevations
Pericarditis: The hallmark features of pericarditis are diffuse global concave ST elevations with associated PR depressions. Patients with pericarditis will classically have chest pain that is worse with laying back and improved by sitting forward. Pericarditis itself may not cause instability, but an acute and/or large percardial effusion may cause pericardial tamponade.
The ECG findings of pericarditis are:
Diffuse ST-segment elevations
PR depressions, classically best seen in leads II and V6
ST Depression in lead AVR
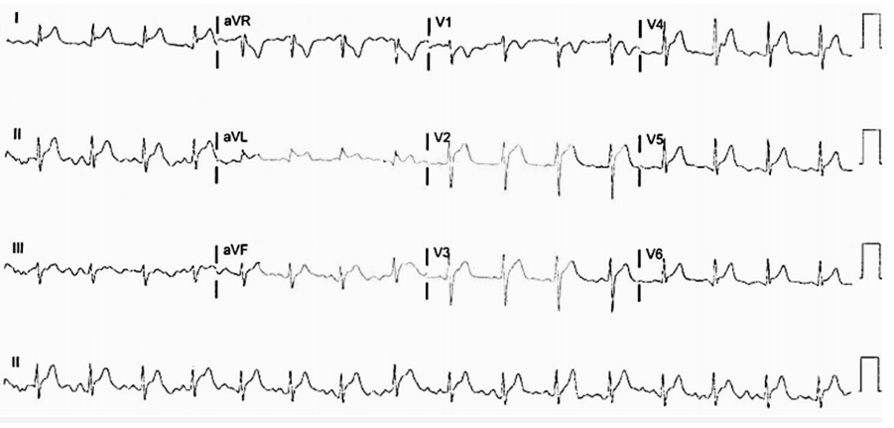 Figure 21. Pericarditis ECG with diffuse ST elevations with PR depressions in lead II. Please also note the ST depression in AVR. Image courtesy of Navdeep Sekhon,
MD.
Figure 21. Pericarditis ECG with diffuse ST elevations with PR depressions in lead II. Please also note the ST depression in AVR. Image courtesy of Navdeep Sekhon,
MD.
Left Bundle Branch Block (LBBB): LBBB does signify underlying heart disease but may be new or a chronic change. LBBB is caused by blockage of the left segment of the Bundle of His and causes ventricular depolarization to occur in a right to left direction (as opposed to the normal left to right). This in turn causes QRS prolongation (>120 ms) and an abnormally appearing QRS complex. Leads V1-3 will have deep S waves and V5-6 will have tall R waves. Diagnosing a patient with a STEMI in the setting of LBBB is challenging as the traditional STEMI definition cannot be used. It is recommended to consult a clinical decision rule such as the Sgarbossa criteria (as described above) to diagnose a STEMI in the context of LBBB on ECG. In the past, a new LBBB in a patient with ischemic chest pain was considered to be an indication for a patient to undergo cardiac catheterization. However, in recent years this has become more controversial with evidence suggesting these patients may be managed more conservatively
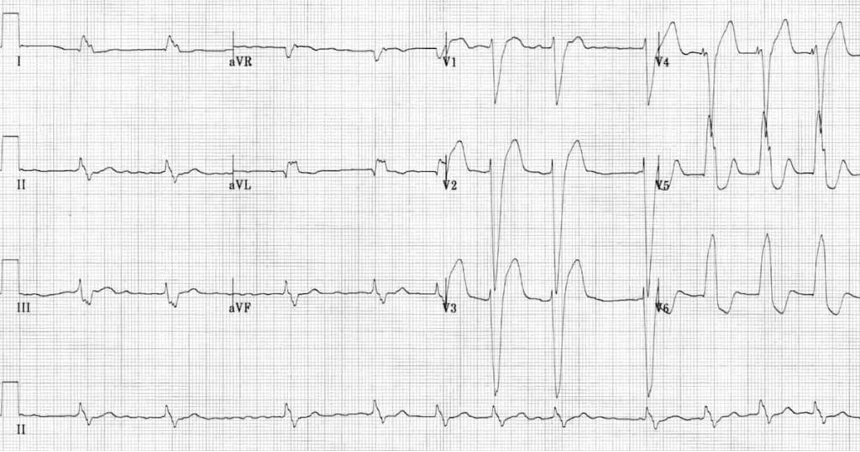 Figure 22. ECG demonstrating Left Bundle Branch Block. Courtesy of Life in the Fast Lane and used under the Creative Commons Attribution-NonCommercial-ShareAlike
4.0 International License. The original image can be found on: Left Bundle Branch Block (LBBB) • LITFL • ECG Library Diagnosis.
Figure 22. ECG demonstrating Left Bundle Branch Block. Courtesy of Life in the Fast Lane and used under the Creative Commons Attribution-NonCommercial-ShareAlike
4.0 International License. The original image can be found on: Left Bundle Branch Block (LBBB) • LITFL • ECG Library Diagnosis.
Common Benign Causes ST elevation
Ventricular Paced Rhythm: A paced rhythm on ECG will appear morphologically similar to LBBB (see above) with discordant ST elevations seen. The one noticeable difference will be the presence of pacer spikes. You cannot use the traditional STEMI definition to detect STEMI’s in a paced rhythm, and you have to rely on tools like the Sgarbossa Criteria.

Figure 23. ECG with Dual Chamber pacing. Courtesy of Life in the Fast Lane and used under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The original image can be found on: Pacemaker Rhythms – Normal Patterns • LITFL • ECG Library Diagnosis.
Benign Early Repolarization (BER): Benign early repolarization usually represents a normal variant most often seen in young, healthy patients. Concave ST elevations are most prominent in leads V2-5 and there is often a “fish hook” or notching at the J-wave in lead V4. The ST changes in early repolarization may be more prominent at slower heart rates and resolve with tachycardia. Caution should be used in diagnosing BER in older patients.
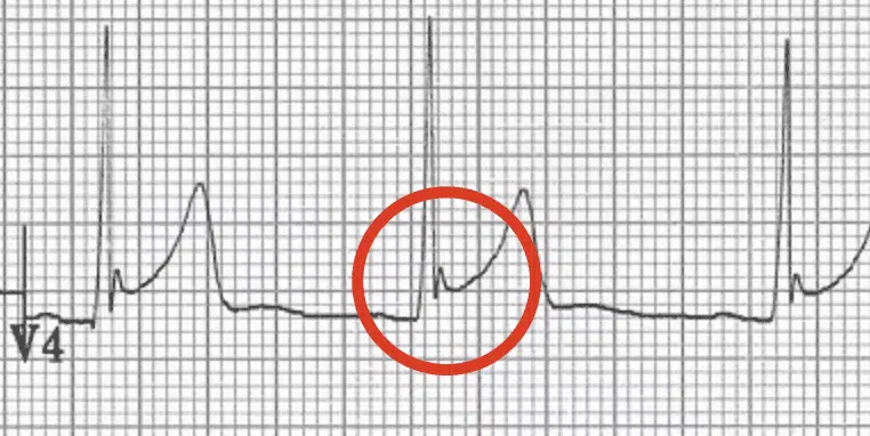
Figure 24. Notching of the J point in Benign Early Repolarization. Courtesy of Life in the Fast Lane and used under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The original image can be found on: Benign Early Repolarisation • LITFL • ECG Library Diagnosis.
Left Ventricular Hypertrophy (LVH): LVH causes a similar pattern of ST elevations as LBBB with ST elevations present in leads with deep S waves (V1-3) and ST depressions or T wave inversions present in leads with tall R waves (I, AVL, V5-6). The ECG changes that are seen are due to thickening of the left ventricular wall leading to prolonged depolarization.
Treatment
Rapid treatment of a STEMI is essential to minimizing morbidity and mortality. In the Emergency Department, arranging for prompt reperfusion therapy is paramount.
For STEMIs, reperfusion usually takes place in the form of percutaneous coronary intervention (PCI) or thrombolytics. For Emergency Departments that have on-site PCI capability, PCI is preferred and the goal Door to Balloon time is less than 90 minutes.
If an Emergency Department does not have on-site PCI capability, they should be transferred for emergent PCI if the expected Door to Balloon time is less than 120 minutes. If the expected Door to Balloon time is greater than 120 minutes, then the patient should receive thrombolytic therapy (tissue plasminogen activator, for example) in the Emergency Department. For patients receiving thrombolytics, the goal Door to Needle time for administering the thrombolytics is less than 30 minutes.
For patients receiving PCI, the following medications can be given in the Emergency Department before the patient goes for their PCI:
Aspirin
Anticoagulation (unfractionated heparin vs low molecular weight heparin vs bivalirudin). Please consult your local cardiologist for your local hospital’s preferred regimen
Clopidrogel or ticagrelor: This is institution-dependent and some institutions prefer to give this after the PCI.
Pearls and Pitfalls
Not all STEMIs have ST Elevation. A classic example is the posterior STEMI which can present with ST-depressions in the anterior leads and De Winter’s T-waves.
Not all STEMIs present with chest pain, but can present with symptoms such as nausea, vomiting, epigastric pain, and weakness. It is important to maintain a high index of suspicion to not miss this important diagnosis.
Rarely, STEMIs can be caused by an aortic dissection. Make sure that you have a high index of suspicion and do not prematurely anchor on the STEMI found on the ECG.
Case Study Resolution
You walk into the room and quickly recognize that the patient is having an inferior STEMI with complete heart block (third degree heart block).
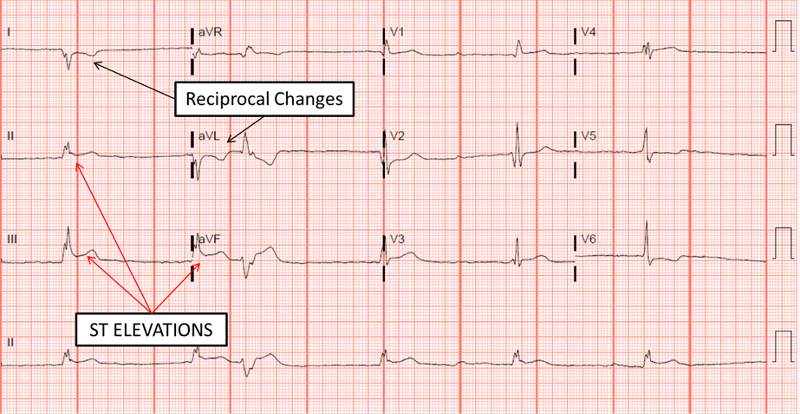
Figure 25. Inferior STEMI with complete heart block. This patient had 100% occlusion of the Right Coronary Artery. After stenting, the patient went back into sinus rhythm. Image courtesy of Navdeep Sekhon, MD.
Code STEMI is activated and the Interventional Cardiologist arrives 20 minutes later to whisk the patient away to the cath lab. In the Emergency Department, the patient receives aspirin, plavix, and heparin. For her hypotension, the patient receives one liter of intravenous fluid and is transcutaneously paced with an improvement of her blood pressure to 100/60 mmHg.
The cardiac catheterization demonstrates an acute 100% RCA (right coronary artery) lesion and the vessel is stented. Post PCI, the third degree heart block resolves and the patient is discharged two days later from the hospital.
References
Gersh BJ, Stone GW, White HD, Holmes DR. Pharmacological Facilitation of Primary Percutaneous Coronary Intervention for Acute Myocardial Infarction: Is the Slope of the Curve the Shape of the Future? JAMA. 2005;293(8):979–986. doi:10.1001/jama.293.8.979
Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003 Jan 4;361(9351):13-20. doi: 10.1016/S0140-6736(03)12113-7. PMID: 12517460.
Kontos M, de Lemos J, et al. 2022 ACC Expert Consensus Decision Pathway on the Evaluation and Disposition of Acute Chest Pain in the Emergency Department. J Am Coll Cardiol. null2022, 0 (0) . https://doi.org/10.1016/j.jacc.2022.08.750
Lawton, Jennifer S et al. “2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines.” Journal of the American College of Cardiology 79.2 (2022): e21–e129. Web.
Lizzo JM, Chowdhury YS. Posterior Myocardial Infarction. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553168/
Sgarbossa EB, Pinski SL, Barbagelata A, et al. Electrocardiographic Diagnosis of Evolving Acute Myocardial Infarction in the Presence of Left Bundle-Branch Block. http://dx.doi.org/101056/NEJM199602223340801. 2009;334(8):481-487. doi:10.1056/NEJM199602223340801
Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019;40(3):237-269. (Guideline) DOI: 10.1093/eurheartj/ehy462
