Headache
Pediatric Headache
Michael D. Parsa, MD
Paul L. Foster School of Medicine Texas Tech University Health Sciences Center, El Paso
Objectives
After reading through this document carefully the reader should be able to:
- Identify pediatric patients presenting with headache that are at high risk for life-threatening complications
- Understand and explain the initial diagnostic approach to a pediatric ED patient presenting with headache
- List the emergent differential diagnoses for pediatric headache
- List the most common discharge diagnoses in pediatric patients presenting to the ED with headache
- List clinical manifestations that raise concern for a brain tumor in pediatric headache
Initial Actions and Primary Survey
First, look at the vital signs and determine which ones are abnormal. Fever? Infection becomes more likely. Significantly elevated blood pressure? Think about hypertensive crisis. Tachycardia? Possibly the patient is in pain. Bradypnea? This could be secondary to elevated intracranial pressure, however, this would not be an isolated finding, but would be associated with a decreased level of consciousness. Hypoxia? Regardless of etiology, this can cause headache, especially if it is of recent onset.
Second, read the triage note. What other signs and symptoms are noted by the nurse? Is the child active and appropriate? If the triage note suggests anything concerning proceed immediately to assess the patient.
Third, when you walk into the room, observe how the patient is acting. Are they playing, drinking or eating? Are they comfortable in their parent’s arms? Make sure the patient is not in distress, exhibiting lethargy or altered mental status. If the child appears generally stable consider symptomatic treatment with ibuprofen or acetaminophen. Consider an age-appropriate antiemetic if nausea or vomiting are present.
Fourth, take a history and ask about associated symptoms such as fever, neck pain or vomiting. Vomiting is especially concerning if it is progressive and is not associated with other gastrointestinal symptoms. Is there photophobia or other visual changes? Are there changes in behavior or mental status that the parents may have noticed? Has the headache happened before? If so, delve into this history further including frequency, severity, character and progression. Did the patient have seizure-like activity? Suspicion for intracranial mass should be high with a first time seizure. A focal seizure could help localize brain involvement. Other indicators of intracranial mass would be a headache that is worse in the morning or when lying down, nighttime awakening from headache, occipital headache, hearing problems, diplopia or if they have been happening for a few weeks or months and are increasing in frequency and severity.
During your history be sure to identify patients who have high-risk conditions.
Preceding trauma? – Decision rules are available to assist in determining which minor head injury patients will need a head CT (see references 1-2).
Blood dyscrasia? Any coagulopathy, hemophilia, thrombocytopenia or sickle cell disease patient would be at high risk for intracranial hemorrhage. Sickle cell disease patients are also at high risk for vascular occlusion causing cerebral infarct.
VP shunt? VP shunt obstructions present with one or more of the following: headache, vomiting, altered mental status, or ataxia. If any of these are present in a child with a VP shunt the shunt may be obstructed. (Figure of VP shunt) This child would be at risk for cerebral herniation and a head CT is warranted to exclude shunt obstruction.
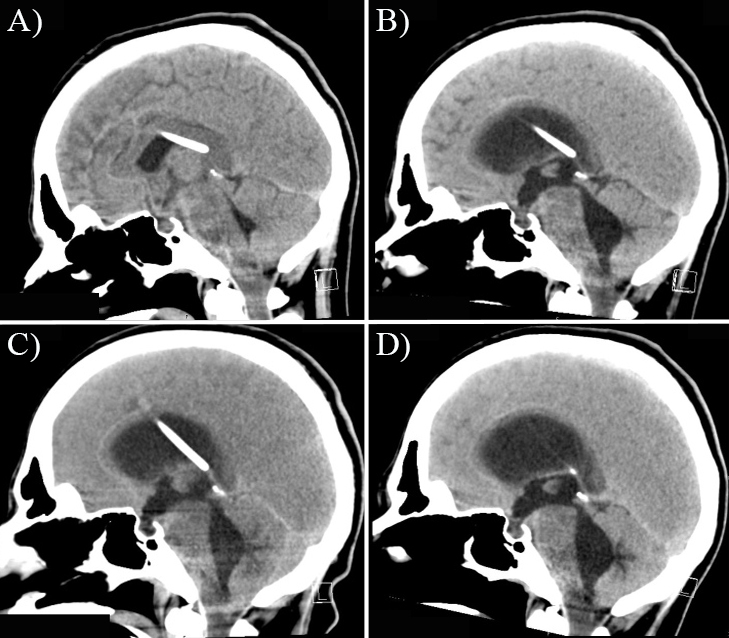
CT demonstrates hydrocephalus secondary to shunt obstruction
Immunocompromised? Children with SCID’s (severe combined immunodeficiency), acquired (post-infectious, drug induced) versus immune (autoimmune, chronic idiopathic, cyclic) neutropenia, asplenia (functional: sickle cell patients and traumatic) are at higher risk for CNS infection, especially brain abscess.
Cancer patient? Higher risk for infection or hemorrhage and may also have metastatic disease.
Cyanotic heart disease? Patients with a persistent right to left shunt are at higher risk for brain abscess (Figure) than the general pediatric population. This is because any venous bacteremia might not be filtered out by the pulmonary circulation. Clinicians should have a low threshold for ordering a head CT when they present with headache.
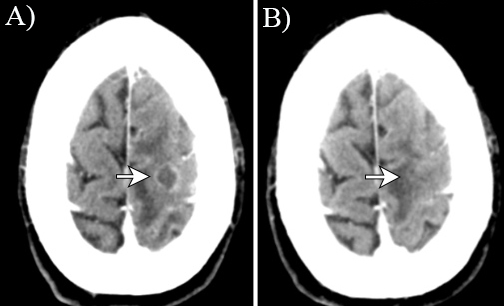
Brain Abscess
Ask about events surrounding the onset of the symptoms. Are there other family members with similar symptoms? If so, consider carbon monoxide poisoning, especially if there is recent onset of cooler weather and use of heaters.
Finally, examine the child. Focus on areas of most relevance after your history. If the child has a history of trauma look for signs of injury. Blood disorder? Look for evidence of bleeding, petechial lesions or bruising. Fever? Look for signs of infection or limited neck movement due to pain.
For all patients do a complete neurologic exam. Assess mental status, cranial nerves, fundoscopic examination, motor and sensory function in the extremities, reflexes, cerebellar testing and ambulation, as appropriate for age.
Unilateral pupillary dilation would be concerning for uncal herniation, in conjunction with a decreased level of consciousness. Papilledema on fundoscopic exam would indicate elevated intracranial pressure. Altered mental status, changes in activity levels and changes in behavior should raise concern for a more serious etiology such as a CNS infection. Any new focal neurologic deficit requires neuroimaging and is most commonly of very serious origin such as mass or hemorrhage.
Differential Diagnosis
Emergent conditions, though uncommon, MUST be excluded prior to discharging a patient home. This can usually be done by history and physical alone.
Emergent conditions:
- Traumatic brain injury, other than concussion
- Ventriculoperitoneal shunt obstruction
- CNS infections
- Carbon monoxide poisoning
- CNS mass lesion
- Intracranial hemorrhage
- Hypertensive crisis
Most common discharge diagnoses in pediatric patients presenting to the ED with headache:
- Viral upper respiratory infection
- Otitis media
- Sinusitis
- Dental infections
- Pharyngitis (especially due to strep)
- Migraine
- Tension headache
- Concussion
References
- Gabor D. Kelen, J. Stephan Stapczynski, et al. Emergency Medicine: A Comprehensive Study Guide, 7e: 880-884
- Giza CC, Kutcher JS, Ashwal S, et al. Evidence-based guideline update: Evaluation and management of concussion in sports. Report of the Guideline Development Subcommittee of the American Academy of Neurology. American Academy of Neurology, 2013. Available at: http://www.neurology.org/content/early/2013/03/15/WNL.0b013e31828d57dd.full.pdf. Accessed November 6, 2014
- Honig PJ, Charney EB. Children with brain tumor headaches. Distinguishing features. Am J Dis Child 1982; 136:121.
- http://www.mdcalc.com/pecarn-pediatric-head-injury-trauma-algorithm/
- King, Christopher. Emergent evaluation of headache in children. In: UpToDate, Fleisher GR (Ed), UpToDate, Waltham, MA (Accessed on November 5, 2014)
- Kan L, Nagelberg J, Maytal J. Headaches in a pediatric emergency department: etiology, imaging, and treatment. Headache 2000; 40:25.
- Kupperman N, Holmes, JF, Dayan PS, et al: Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet 374 (9696): 1160, 2009.
- Schultz BRE, Macias CG, “Chapter 130. Headaches in Children” in Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. 2010.
