Acute Coronary Syndromes
Author: Eric Blazar, MD, Inspira Medical Center, Rowan University,
Editor: Dan Mayer, MD, FAAEM, FACEP, Niskayuna, NY
Last Update: September, 2019
Case Study
Case study: A 74-year-old male presents to the ED from home complaining of chest pain. Upon further questioning he states he was watching a baseball game in his recliner when his pain started. He describes the pain as pressure over the left chest that started 45 minutes prior to arrival. The pain radiates to the right arm and is associated with some nausea but no vomiting. He denies shortness of breath or diaphoresis. He states that he usually gets this pain with exertion and it is usually relieved with his home nitroglycerin. He states he took 3 nitro at home without improvement of his symptoms. His wife then brought him in for evaluation. She states he has a history of coronary artery disease, DM type II and hypertension. His vital signs are within normal limits except his pulse is 110 bpm. His physical examination is unremarkable. An EKG is appropriately obtained immediately upon arrival interpreted by the clinician as sinus tachycardia with inverted T waves with 1 mm of ST depression in leads II, III and aVf. What interventions are necessary immediately? What distribution of the heart is affected? What diagnostic tests are necessary?
Objectives
Upon finishing this module, the student will be able to:
- Discuss the continuum of disease in acute coronary syndromes.
- Understand the necessary immediate diagnostic work up and treatment for ACS patients.
- Risk stratify patients with chest pain suspected for ACS in the ED.
- Identify indications for emergent PCI
- Interpret EKG lead “families”
Introduction
Chest pain is the leading complaint for ED visits in the United States (estimated 5-8 million presentations annually). Acute coronary syndrome (ACS) represents the continuum of disease representing decreased coronary blood flow and acute myocardial ischemia and/or infarction. This decreased flow is abrupt in nature. The ACS continuum consists of unstable angina, non-ST elevation myocardial infarction (NSTEMI) and ST elevation myocardial infarction (STEMI). ACS is a mix of reversible and irreversible cardiac ischemia. The large majority of patients that come to the ED with chest pain, will not have ACS but it is also the responsibility of the emergency physician to risk stratify chest pain patients for having cardiac events one of the many emergent etiologies that can present with chest pain (only about 25% of all chest pain ED visits). The emergency physician must also consider other emergent etiologies causing chest pain such as: pneumonia, aortic dissection, pneumothorax, esophageal ents (MACE: Major Adverse Cardiac Events; all cause mortality, myocardial infarction and coronary revascularization) in their short term future. ACS represperforation and pulmonary embolism.
Initial Actions and Primary Survey
Patients with chest pain tend to arrive by both private vehicle and EMS transport. Many critical actions and assessments must occur early in presentation. Chief amongst them is an EKG, which should be obtained immediately (<10 minutes) to rule out ST elevation MI (STEMI). ABCs should be evaluated for adequate oxygenation and circulation, and an initial history of the pain and associated symptoms should be obtained. A primary survey should include an initial examination of the neck (for distended neck veins), heart, lungs, abdomen (for enlargement of the liver or spleen), and extremity examination for circulation and edema. The patient should have an IV placed and be placed on a continuous cardiac monitor. If the physician does not suspect an acute aortic dissection, 324 mg of chewable aspirin should be given. If there is any suspicion of an acute coronary syndrome, labs including blood count, electrolytes, cardiac enzymes, a chest radiograph and repeat EKGs will also be ordered.
Presentation
The classic description of cardiac chest pain is an intermittent, substernal chest pressure, usually on the left which radiates to the arm and neck, exacerbated with exertion and associated with shortness of breath, diaphoresis, nausea and palpitations/lightheadedness. It is often associated with patients that have a history of smoking, CAD, hypertension and diabetes mellitus.
Just as common as “typical” presentations of ACS are “atypical” presentations. Atypical presentations commonly occur more frequently in women, diabetics and elderly. The pain can occur anywhere from the umbilicus to the neck and to the back. It can be sharp, burning (simulating gastric reflux) or only be associated with mild “discomfort”. Diabetics and the elderly may have no chest pain at all. Women often present simply with fatigue, shortness of breath and generalized weakness.
The continuum of cardiac chest pain starts with stable angina (unchanged exertional pain lasting 5-15 minutes and relieved by rest or nitroglycerin). Unstable angina (increasing in frequency, at lower exertional levels, occurs at rest or unrelieved by rest or nitroglycerin) is the beginning of the ACS continuum. The spectrum, encompassing NSTEMI and STEMI, is quite dynamic and may lead to MI or death.
The physical exam can also be highly variable. Patients often appear normal in appearance, or may be in full cardiac arrest. They may be diaphoretic, hypotensive or hypertensive, tachycardic or bradycardic, or dyspneic. They may have normal heart sounds, or a murmur from the rupture of a papillary muscle or valve. There may be signs of heart failure (third heart sound, JVD, pedal edema, pulmonary edema). The importance of a good history and physical examination cannot be stressed enough as the basis for making this diagnosis.
Variability in presentation makes ruling out an ACS by history and physical examination alone very difficult. Pretest probability (risk stratification) will increase and decrease based on presence or absence of “classic findings”. However, ruling out ACS on history and physical alone is not advised or founded in current research.
Diagnostic Testing
Diagnostically, there are two major goals for patients presenting to the ED with chest pain. The first goal is to rule in an acute MI (STEMI/NSTEMI) or other emergent reason for the need for cardiac intervention. The second is to risk stratify patients for future coronary events.
Acute Myocardial Infarction (MI)
An acute MI is diagnosed by satisfying two of the following three criteria:
- Clinical history consistent with ACS
- EKG changes
- Elevation in troponin enzymes
Clinical History
ST elevation MI is defined as:
- New ST segment elevations in at least two anatomically contiguous leads:
- Men age >40 years: >2 mm in V2-V3 and >1 mm in all other leads
- Men age <40 years: >2.5 mm in V2-V3 and >1 mm in all other leads
- Women (any age): >1.5 mm in V2-V3 and >1mm in all other leads
EKG‘s are the essential screening tool for patients with chest pain. ST segment elevations are highly concerning for acute MI and are present in 40% of acute MIs. However, other less specific findings are quite frequent. Other signs to look for on EKG are hyper-acute T waves, ST segment depressions, inverted T waves and new conduction abnormalities. Always attempt to compare the current EKG to a patient’s old EKG. Serial EKGs can be key in diagnosing acute MI, looking for dynamic changes throughout a patient’s ED course.
Noting the leads affected with ST changes can localize an acute occlusion (Figure 1). The traditional 12-lead EKG does not easily detect posterior and right-sided MIs. Look for reciprocal changes on any EKG such as ST-depressions in leads on the opposite side of the affected coronary occlusion. These reciprocal changes are negative deflecting electricity on the opposite side of the heart from the acute occlusion. If there is concern for right sided or posterior MI, specific EKGs with different lead placement can be obtained (V7, V8, V9 for posterior; V4R, V5R, V6R for right sided). Usually EKG geography is related to specific coronary anatomy (ie inferior STEMI correlates with blockage in the right coronary artery or RCA branch).
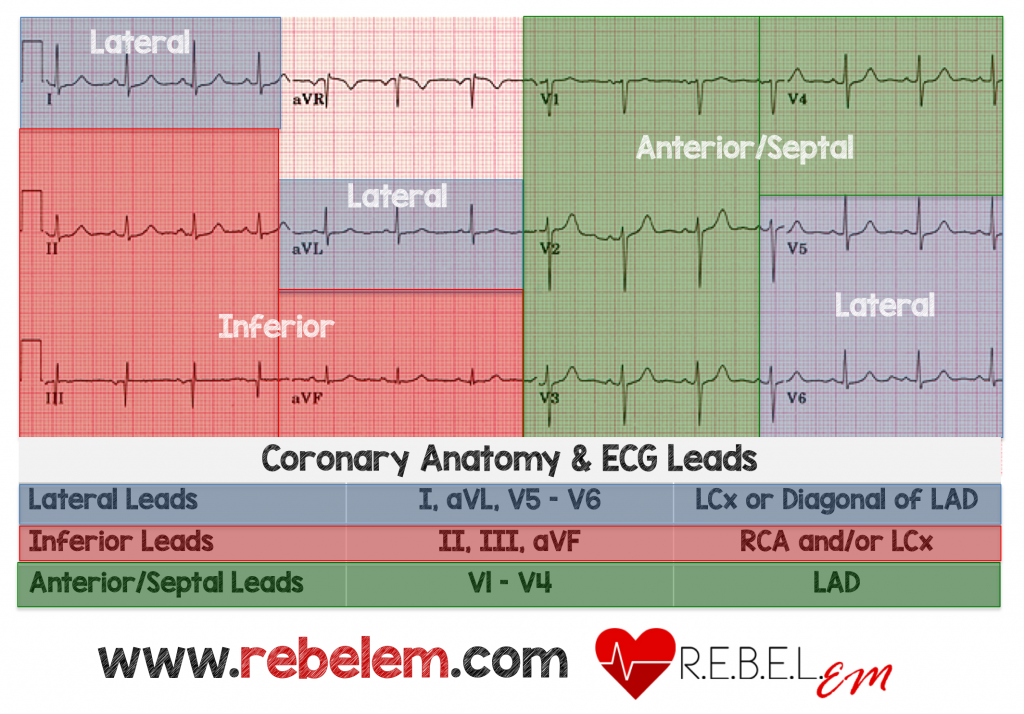
Figure 1: Typical locations of infarction or ischemia based on EKG leads with abnormalities (ST elevation for STEMI or depression and T-wave inversion for ischemia, UA or NSTEMI). Source: Chest Pain, “Negative” Stress Tests, POCUS, & ECG Equations, RebelEM found at: https://rebelem.com/chest-pain-negative-stress-tests-pocus-ecg-equations/. Used under the Creative Commons License http://creativecommons.org/licenses/by-nc-nd/3.0/deed.en_US

Figure 2. Life in the Fast Lane Used under the Creative Commons License http://creativecommons.org/licenses/by-nc-nd/3.0/deed.en_US
Figure 2 displays an anterior STEMI evidenced by elevations in V2-V4 with reciprocal depression laterally

Figure 3. Life in the Fast Lane Used under the Creative Commons License http://creativecommons.org/licenses/by-nc-nd/3.0/deed.en_US
Figure 3 shows elevations in lead I and aVL with reciprocal changes inferior.

Figure 4. Used under the Creative Commons License http://creativecommons.org/licenses/by-nc-nd/3.0/deed.en_US
Figure 4 shows an inferior STEMI (elevations in II, III and aVF) with reciprocal ST depressions laterally. Reciprocal changes are negative electric deflections usually on the opposite side of the heart from the occluded vessel.
Enzyme testing is another staple of ACS diagnosis and risk stratification. Cardiac enzymes are specific to myocardium and released in episodes of stress such as inadequate blood flow to the myocardium. Elevated enzymes alone are not specific for MI. These enzymes are often “trended” or obtained at multiple time points. Often times, depending on the lab test being ordered, there is a delay from the acute occlusive event to enzyme detection in the blood. In the past, CK, myoglobin and CK-MB levels were checked along with classic troponin. However, these tests have proven to be less useful and are no longer ordered in the laboratory evaluation of ACS. Troponin assays vary (troponin T, I, high sensitivity) and the normal ranges are institution specific.
NSTEMI
Patients that have EKGs that do not meet the above discussed STEMI criteria but have ischemic changes (ST depressions, T wave inversions or hyperacute T waves, Figure 5) and/or positive troponins are classified as non-ST segment elevation MIs (NSTEMI). The acute management of these patients involves relief of ischemic pain, maintaining/correcting hemodynamics (tachycardia and hypertension will increase O2 demand), antithrombotic therapy as well as management strategy. These patients are frequently treated with anticoagulation as well as an antiplatelet medication. As opposed to STEMI patients, there is no benefit from fibrinolysis or emergent angiography/revascularization. Immediate angiography and revascularization has only shown benefit in patients with hemodynamic instability/shock, severe LV dysfunction, persistent rest angina, mitral regurgitation or sustained ventricular arrhythmia. Patients with an NSTEMI tend to be older and have more comorbidities than compared to patients with STEMI.

Figure 5. Life in the Fast LaneUsed under the Creative Commons License http://creativecommons.org/licenses/by-nc-nd/3.0/deed.en_US
NSTEMI vs. STEMI
Differentiating between STEMI and NSTEMI becomes very important as acute ED management changes. Extensive research has shown that STEMI patients benefit from emergent revascularization/stenting/PCI. This benefit has been born out in that STEMI on EKG usually represents an acute occlusion of a major vessel. Research in NSTEMI patients has not shown benefit and in fact, has shown potential harm from emergent PCI. Non-emergent PCI in NSTEMI patients has shown long term benefit in preventing non-fatal MIs but patient oriented outcomes have shown no advantage. NSTEMI patients tend to have reversible or non-total occlusive disease.
As previously discussed, ED diagnosis of acute ACS/MI is based on clinical history and exam, EKG and cardiac biomarkers. However, if these initial tests are negative, the patient’s chest pain can still be related to MI. In situations where ACS is suspected, additional troponins and serial EKGs should be obtained to further decrease the likelihood of acute MI.
So what if all of the testing is negative?
As previously noted, MI is not entirely excluded by an initially negative EKG and normal biomarkers. Diagnosing an MI with a positive EKG or positive troponin is straightforward. What is more challenging is the patient who has a non-diagnostic EKG and normal cardiac biomarkers. Risk stratification can help in determining the need for admission with immediate further cardiac testing or discharge home for outpatient followup.
Risk stratification
In the ED, as physicians, we are also responsible for the patient’s short-term future. Patients presenting to the ED with chest pain who have a low likelihood of acute MI are still to be evaluated for the remainder of the ACS continuum. This represents likely the most difficult part of evaluating chest pain patients in the ED.
How can an MI be “ruled out” in the ED?
Overall, there is no method to guarantee that MI is “ruled out” in the ED. Utilizing risk scores and delta troponins we are able to assess a patient’s short term risk for ACS/MI in the short term.
In order to aid in this risk stratification, many risk scores and calculators have been utilized to assess for short-term morbidity and mortality. Classically, the TIMI score or others were used. More recent, the HEART score, uniquely developed in emergency department patient populations, has been validated and become more useful in clinical practice. The HEART score, which can be accessed using an on-line calculator (https://www.mdcalc.com/heart-score-major-cardiac-events) is used to risk stratify patients. History, EKG, Age, Risk factors and Troponin (HEART) are all assigned points and can calculate the risk as low, moderate and high-risk for MACE. Classically, patients stratified as low-risk have a 0.9-1.7% risk of MACE at 6 weeks. If a second troponin three hours later is negative and unchanged from the first value, the patient can be discharged home for outpatient followup with a cardiologist or primary care physician. Moderate-risk MACE is 17% at six weeks and high-risk patients have a MACE is 50%. These latter two risk groups should be admitted to the hospital. While hospitalized either as an inpatient or observation telemetry patient, a combination of cardiology evaluation, dynamic testing (stress, echo, CT coronary) and continued timed serial troponin testing is performed. The treatment and stratification of chest pain in the emergency department is an ever-changing practice, where the ED physician is constantly balancing risk and benefit to the patient. The EDACS score is another frequently used risk stratification tool that performs similarly to the HEART score. It is longer than HEART and has slightly better specificity. Both are available in on-line calculators.
The idea of sending a second troponin is known as a Δ troponin. A second troponin is measured to monitor changes in a troponin value over time. As there is significant lag between an ischemic event and measurable change in troponin, often times monitoring the change in a troponin over a specific time period aids in risk stratification. Usually a Δ troponin is measured at 2 or 3 hours following initial troponin measurement. Usually a low-risk HEART score combined with negative 2-3 hour Δ troponin can be discharged to home with expeditious primary or cardiology follow up. However, always take into account the patient’s story and access to follow up as well as other factors that can influence patient care.
The American Heart Association’s current recommendation from 2010 states that all chest pain patients discharged from the ED must undergo provocative testing (stress, stress echo, etc.) within 72 hours of discharge. This recommendation is the impetus behind placing patients into observation telemetry units. Current practices vary by institution but are moving toward earlier discharge of low and some moderate-risk chest pain patients to allow pursuit of outpatient cardiology follow up and testing.
Treatment
In the emergency department, always place the patient on a cardiac monitor, insert large bore IVs and place the patient on oxygen if indicated by a low oxygen saturation. Aspirin (anti-platelet) is of the utmost important for patients with acute MI. Morphine and nitroglycerin were classically used to decrease a patient’s pain, however, recent studies indicate that morphine may contribute to poorer outcomes (The Death of MONA). Further reading on this topic found on RebelEM blog). Pain improvement with nitroglycerin is consistent with cardiac chest pain but neither sensitive nor specific. Nitroglycerin venodilates and decreases preload and should be avoided in right-sided MIs or if the patient has a low blood pressure (systolic less than 100 mmHg). Beta-blockers are not usually started in the emergency department unless heart rate and blood pressure control is needed.
Once acute MI is identified, there are multiple interventions and treatments pathways. STEMIs and STEMI equivalents go emergently for PCI (percutaneous coronary intervention). Some STEMI equivalents are a new LBBB, a LBBB meeting Sgarbossa’s criteria, Wellen’s waves, ST elevation in aVR, deWinter’s T waves, ongoing presumed cardiac chest pain and out-of-hospital cardiac arrest with STEMI on post-resuscitation EKG.
Both UA and NSTEMI are mostly medically managed. STEMIs should receive maximal medical therapy in the ED prior to undergoing catheterization. Anticoagulation (often heparin) can be started to prevent further coagulation pathway activation. Antiplatelet therapy (aspirin, plavix and IIb/IIIa inhibitors) is also utilized to decrease platelet aggregation. UA and NSTEMI will commonly get urgent catheterization and should be managed in consultation with a cardiologist.
In the absence of immediate access to a cardiac cath lab or if PCI cannot be performed within 120 minutes, thrombolytic therapy is recommended for treatment of STEMI. In the US, tPA is most commonly used.
Pearls and Pitfalls
- Obtain EKG on all chest pain or “atypical” patients and compare to an old EKG if available
- Obtain an initial set of cardiac enzymes
- Risk stratify the patient to determine suitability for Emergency Department evaluation and potential discharge with close follow up
- Obtain serial EKGs and cardiac enzymes
- One negative cardiac enzyme and a normal EKG does NOT rule-out an MI and does not sufficiently decrease patient risk for short term morbidity/mortality
Case Study
Resolution: Upon interpretation of the EKG and remembering the lead families on the EKG, you are very concerned about inferior ischemia. The patient is given an aspirin and started on a heparin drip. Cardiology is consulted for further management. Morphine and a small dose of nitroglycerin are given to attempt pain control. The patient’s blood pressure tolerates the nitro but his pain persists. He is placed on a nitroglycerin drip. His first troponin comes back abnormally elevated at 1.2. Serial EKGs show continued inversions and depressions in the inferior leads. Due to his ongoing and likely cardiac chest pain, he is emergently transferred for PCI. You receive a call 1 hour late from the interventional cardiologist, stating the patient had a stent placed in the right coronary artery and congratulating you on the excellent emergency care you provided for your patient.
FOAM Resources
As emergency cardiology is such a large aspect of EM practice there are many excellent FOAM resources to aid in cardiology learning.
Life In The Fast Lane, litfl.com
https://litfl.com/acute-coronary-syndromes/ provides an in depth ED resource
Dr. Smith’s ECG blog, http://hqmeded-ecg.blogspot.com/ is an excellent further resource for ECG interpretation.
References
- Fanaroff AC, Rymer JA, Goldstein SA, et. al. Does this patient with chest pain have acute coronary syndrome? The rational clinical examination systematic review. JAMA. 314(18):1955-1965
- Herren KR, Mackway-Jones K, Emergency management of cardiac chest pain: a review, Emergency Medicine Journal 2001;18:6-10.
- Mark DG, Huang J, Chettipally U, et. al. Performance of Coronary Risk Scores Among Patients With Chest Pain in the Emergency Department. J Am Coll Cardiol 2018;71(6):606-616.
- McSweeney, Jean C et al. “Women’s Early Warning Symptoms of Acute Myocardial Infarction.” Circulation 2003; 108: 2619-2623.
- Tomaszewski CA, Nestler D, Shah KH, et. al. . From the American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Suspected Non–ST-Elevation Acute Coronary Syndromes: Clinical Policy: Critical Issues in the Evaluation and Management of Emergency Department Patients With Suspected Non–ST-Elevation Acute Coronary Syndromes. Ann Emerg Med; 2018;72:e65-e106
