Pneumothorax
Author: Doug Franzen, MD, M.Ed., University of Washington School of Medicine
Edited by: Benjamin J. Sandefur, MD, Mayo Clinic College of Medicine and Science
Updated: November 2019
Case Study
A 29-year-old male presents to the ED complaining of the sudden onset of left sided chest pain and dyspnea that started while he was playing basketball. He denies any medical problems and takes no medications. He speaks in short sentences as he answers your questions. You note his vital signs: BP 124/68, HR 94, RR 18, sPO2 99% on room air. You have been working on focusing your assessments and considering the questions:. What are the main concerns in this patient? How do you focus your history and exam? What tests will help make the diagnosis? Should any treatments be started prior to definitive diagnostic testing?
Objectives
- Discuss pneumothorax as part of the differential diagnosis of chest pain and/or shortness of breath
- Recognize the common exam findings in patients with a pneumothorax
- Recognize both the radiographic and ultrasonographic findings associated with pneumothorax
- Describe different treatment options for a pneumothorax
Introduction
A pneumothorax occurs when a pleural defect allows the potential space between the parietal and visceral pleura of the lung to fill with air, which subsequently collapses the lung. Pneumothoraces can occur spontaneously or as the result of trauma. They are also a potential complication of multiple procedures and positive pressure ventilation.
Pneumothoraces can be classified as “simple” or “tension.” A simple pneumothorax is non-expanding. In a tension pneumothorax, a “one way valve” defect allows air into but not out of the pleural space. If left untreated, increasing pressure starts to collapse vascular structures within the mediastinum. As pressure builds, venous return to the heart decreases, eventually leading to an obstructive shock state, with hemodynamic collapse and cardiac arrest. Prompt diagnosis and treatment of a pneumothorax is essential.
Spontaneous pneumothorax should be considered in non-trauma patients who complain of dyspnea and/or chest pain. Symptom onset is usually sudden. Other diagnoses that may present similarly to a spontaneous pneumothorax include acute coronary syndrome, thoracic aortic dissection, and pulmonary embolism, as well as pneumonia, pleurisy, and pericarditis. Traumatic pneumothoraces (including iatrogenic) will also present with chest pain and dyspnea, but in temporal proximity to a traumatic event or invasive procedure.
For further discussion of traumatic pneumothorax, see the Chest Trauma section.
Initial Actions and Primary Survey
Before performing a lengthy history and physical examination, the clinician must first consider, diagnose, and treat a tension pneumothorax. Chief complaints of chest pain or shortness of breath suggest pneumothorax. Vital sign abnormalities that increase suspicion for tension pneumothorax include tachycardia, tachypnea, hypoxia and hypotension. Decompensation shortly after the initiation of positive pressure ventilation is highly concerning for an expanding pneumothorax. Breath sounds and respiratory status should be assessed as part of the primary survey. Findings that suggest tension pneumothorax include unequal breath sounds (diminished or absent on the side of the pneumothorax), tracheal deviation (away from the side of the pneumothorax), distended neck veins, and/or signs of respiratory distress. In intubated patients, additional signs of tension pneumothorax include high airway pressures or difficulty bagging.
If signs suggestive of a tension pneumothorax are found, immediate decompression is indicated. Most of the findings noted above are late findings – do not wait for them to appear before taking action.
Presentation
Spontaneous pneumothorax should be considered in patients presenting with dyspnea and/or chest pain. The pain usually begins suddenly and is described as sharp and unilateral, with associated shortness of breath. Patients may also complain of a cough. The pain is often initially pleuritic but may become dull and aching with time. Occasionally the pain is more prominent in the back and shoulder. The degree of dyspnea may increase over time as the pneumothorax increases in size.
A thorough past medical history is important in the evaluation of spontaneous pneumothorax. A spontaneous pneumothorax can be classified as either primary or secondary. A primary pneumothorax occurs in patients that have no underlying pulmonary disease. It is most common in thin, young males with a history of tobacco use. Smoking increases the risk of primary pneumothorax 9-fold in women and 22-fold in men. Cannabis smoking also increases the risk of pneumothorax. A secondary pneumothorax occurs as a result of other underlying disease, most commonly COPD, but also including cystic fibrosis, lung cancer or Marfan syndrome. If the patient has had any recent procedures, iatrogenic pneumothorax should be considered. The most common procedures to cause a pneumothorax include central line placement, thoracentesis, pacemaker placement, tracheostomy, or biopsy. Other causes include CPR and positive-pressure ventilation.
Vital sign abnormalities in patients with pneumothorax can include tachycardia, tachypnea and, depending on the severity, hypoxia and hypotension. Sinus tachycardia is the most common early finding.
In addition to the findings suggestive of tension pneumothorax discussed above, other physical exam findings that can be seen in patients with pneumothorax include diminished or absent breath sounds, hyperresonance with percussion (the side with the pneumothorax will resonate more), asymmetric chest wall excursion (decreased excursion on the affected side), and loss of tactile fremitus on the affected side of the chest. The chest wall should be palpated and any crepitus or signs of trauma should be noted. In addition to a thorough lung exam, look for signs of respiratory distress (nasal flaring, accessory muscle use) and findings suggestive of potential contributing causes, such as nail clubbing.
Diagnostic Testing
As noted above, if tension pneumothorax is suspected and the patient is unstable, proceed immediately to decompression – do not wait for imaging to confirm the diagnosis.
Pneumothorax is classically diagnosed with a chest x-ray. The sensitivity of plain films varies from study to study, from well below 50% to a high of about 80%. Supine films are less likely to detect pneumothorax; upright films improve the sensitivity. A lateral decubitus film is the most sensitive view, able to detect as little as 5mL of air in the pleural space. The classic findings of pneumothorax on chest radiography are a white, visceral pleural line that is parallel to the chest wall, with a loss of vascular lung markings distal to the line, i.e. between the chest wall and the pleural line.
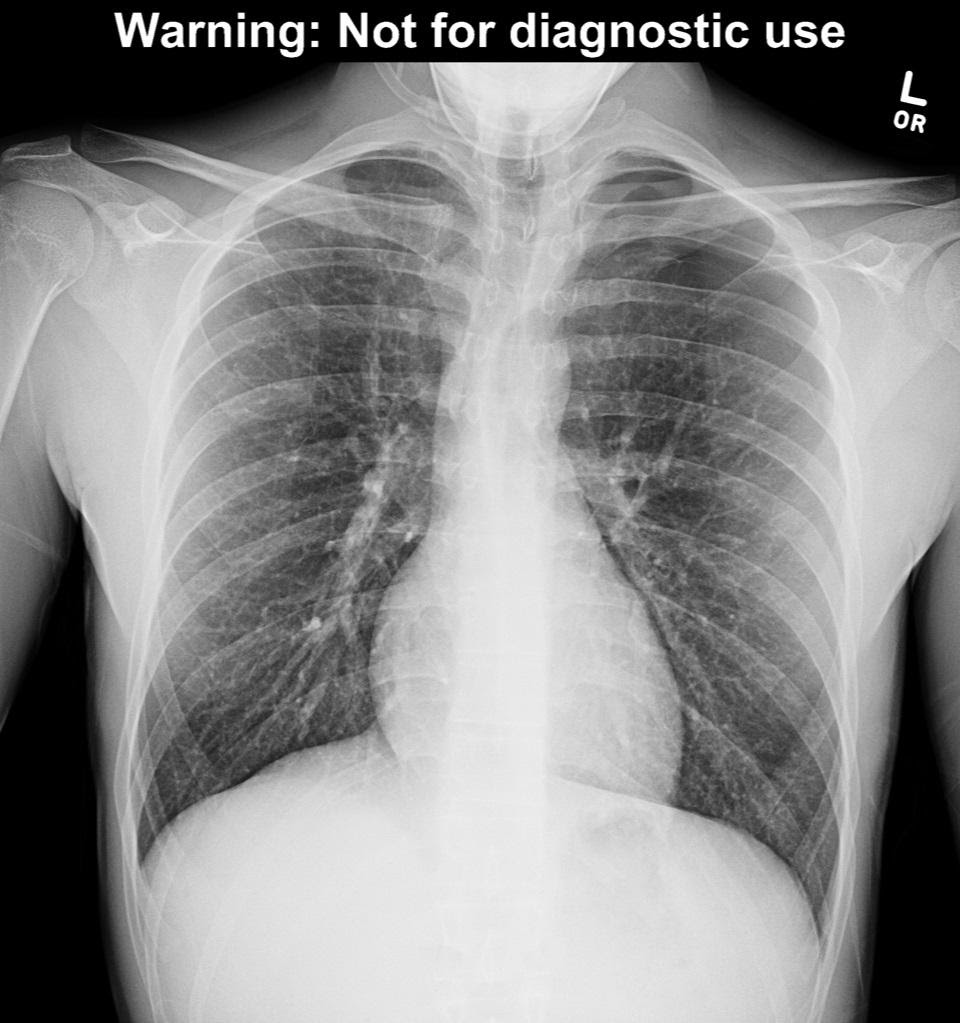
Figure 1a – chest x-ray with pneumothorax. Image used with permission of Joel Gross, MD
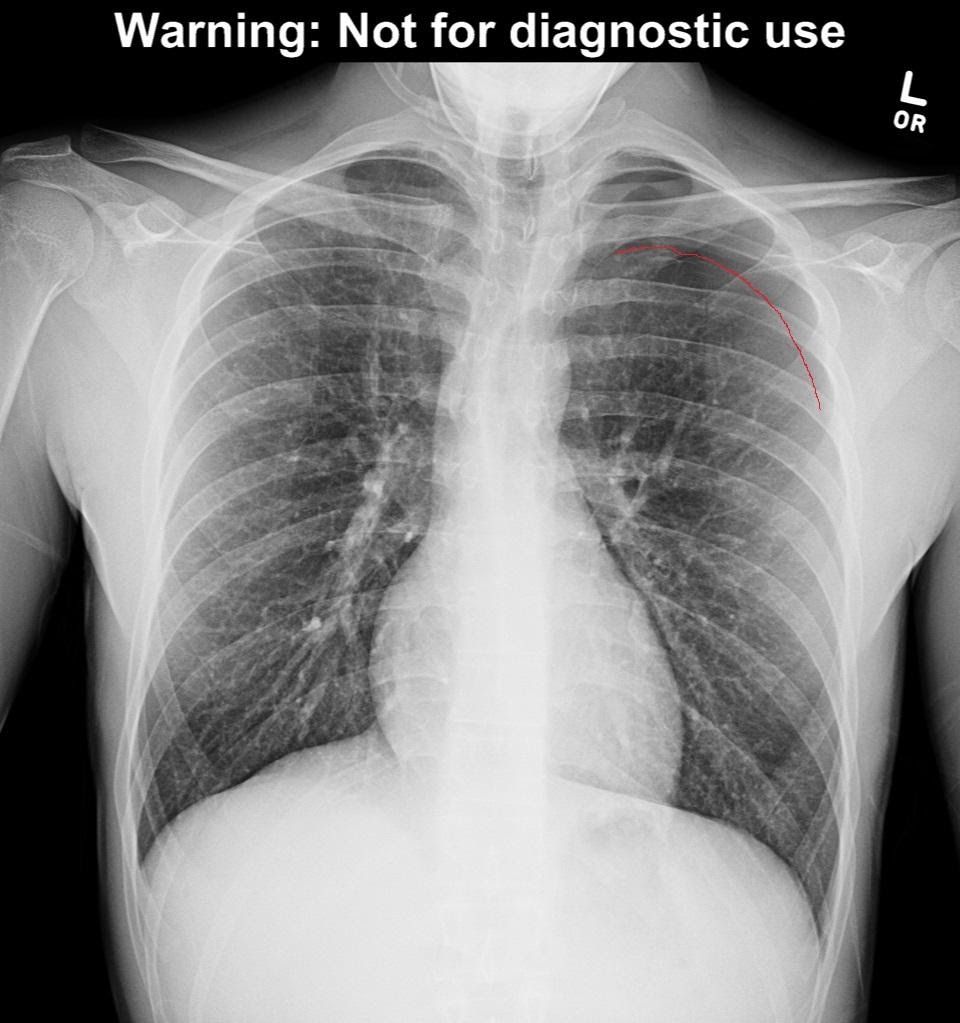
Figure 1b – pleural line highlighted in red, demonstrating left pneumothorax
On a supine film, air layers out across the anterior chest wall and the classic findings above are not seen. Instead, a “deep sulcus” suggests pneumothorax. A deep sulcus is a large, lucent costophrenic angle, extending more inferiorly than expected on the affected side.
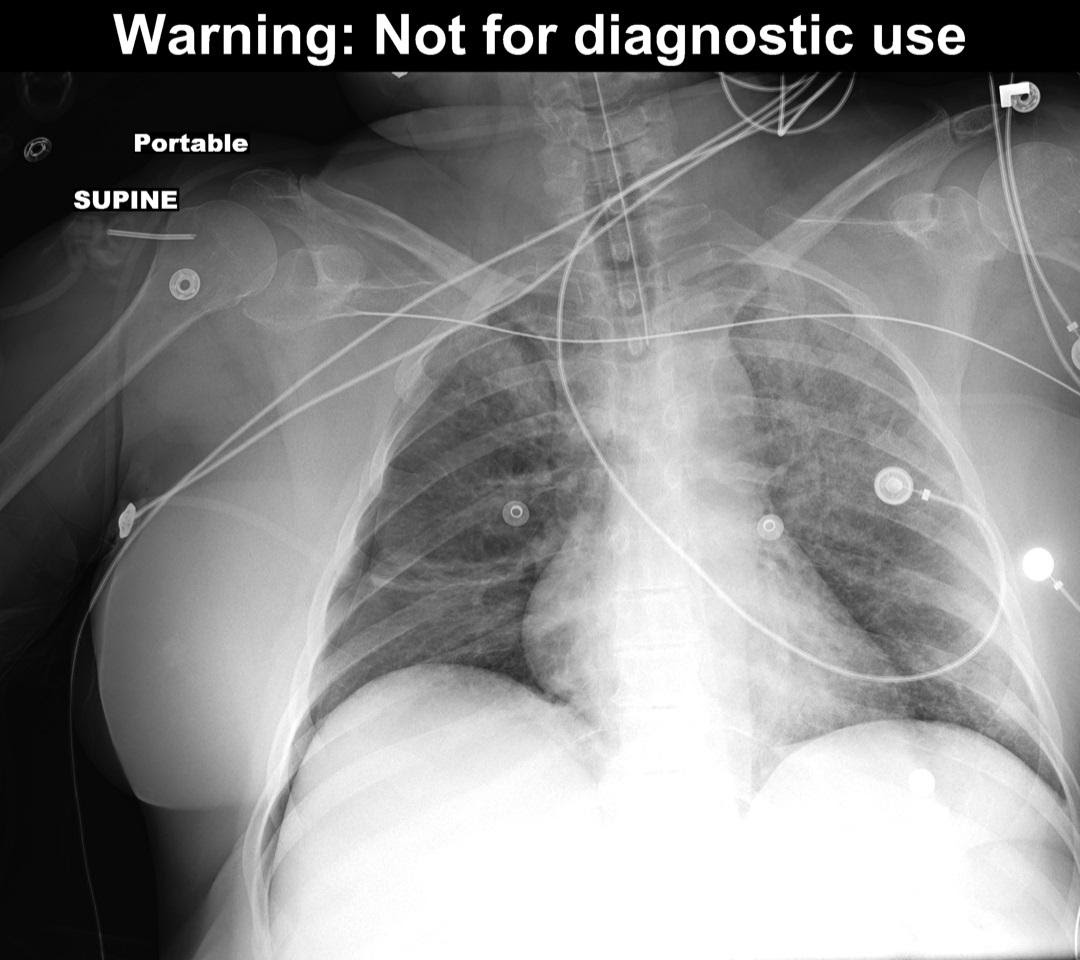
Figure 2 – Deep Sulcus Sign due to right pneumothorax.
Multiple studies have shown that ultrasound is more sensitive than plain films in diagnosing pneumothorax, with the sensitivity of ultrasound approaching that of CT. To evaluate for pneumothorax with ultrasound, have the patient lay supine. Place a linear (vascular/soft tissue) probe in the most anterior point of the chest wall, usually at about the 3rd or 4th intercostal space. The probe should be oriented perpendicular to the ribs (usually marker dot towards the head). A bright white pleural line will be visible just deep to the ribs. In a normal lung you will see the sliding movement of the pleura and a “comet tail” artifact as the patient breathes. These findings are due to the apposition of the two pleural layers. Because air separates the two pleural layers in pneumothorax, absence of these normal findings is diagnostic for pneumothorax.
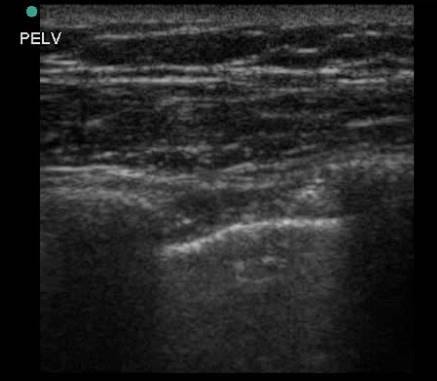
Figure 3 – ultrasound of the anterior chest wall using a linear probe. Note the bright white pleural line visible between and just deep to the ribs. Image used by permission of Doug Franzen, MD
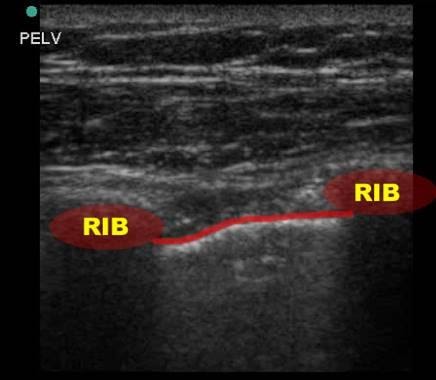
Figure 3a
M-mode can also be used to diagnose pneumothorax. In a normal lung, ultrasound passes through the pleura and the multiple air/tissue interfaces of the alveoli result in a “seashore” appearance. A pneumothorax creates a reverberation artifact beneath the bright pleural line, creating a “bar code” appearance due to multiple bright A-lines.
-vs.-barcode-(pneumothorax---right-image).jpg?Status=Master&sfvrsn=8b2b3319_1)
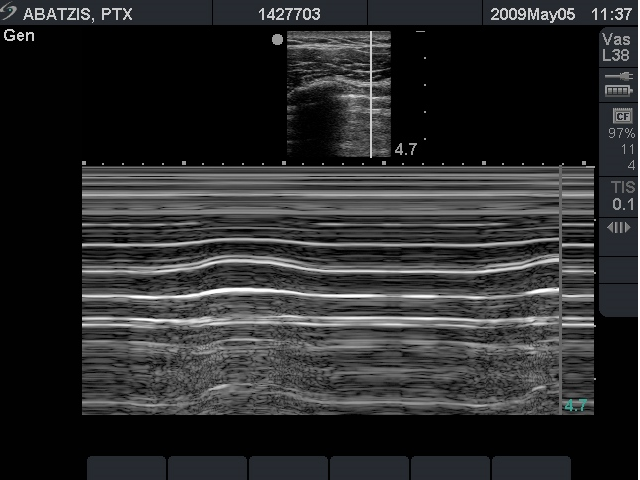
Figure 4 – M-Mode: Seashore (normal - left image) vs. Barcode (pneumothorax - right image)
Images used by permission of Doug Franzen, MD
CT scan is the gold standard for detecting pneumothorax, but is rarely necessary in evaluating spontaneous pneumothorax, as a pneumothorax too small to be detected by other modalities is unlikely to need intervention. More often, a pneumothorax is seen on a CT that has been ordered to evaluate for other processes such as pulmonary embolism when an initial chest x-ray is non-diagnostic. CT can be useful to differentiate between a large bulla and pneumothorax in patients with underlying lung disease.
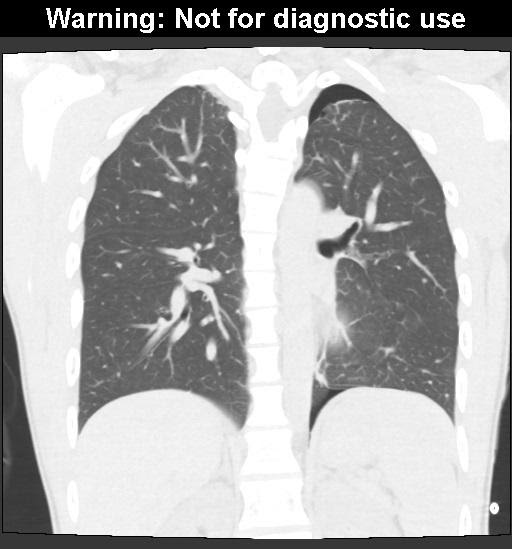
Figure 5 – Pneumothorax as seen on CT
Treatment
Tension pneumothorax should be treated immediately. Needle decompression can be rapidly achieved in most settings. A large-bore (14g) angiocatheter can be placed in either a) the 2nd or 3rd intercostal space at the midclavicular line or b) the 4th or 5th intercostal space at the anterior axillary line. Lateral placement is recommended in obese patients, as the catheter may not be long enough to pierce the pleura in an anterior placement. If needle decompression is performed, the patient will need definitive treatment with chest tube placement.
Once tension pneumothorax has been excluded, the goal of treatment for simple pneumothorax is relief of dyspnea. Management depends on multiple factors, including the degree of symptoms, size and cause of the pneumothorax, and whether this is the first or a recurrent pneumothorax. Multiple different methods have been proposed to estimate the size of a pneumothorax. One of the simplest is measuring the distance from the chest wall to the visible pleural line.
A simple pneumothorax will spontaneously resolve as the air is absorbed. Supplemental oxygen increases the rate of resorption. For small primary spontaneous pneumothoraces (pleural line < 1-2cm from the chest wall) with minimal symptoms, treatment may consist of 100% oxygen applied for a brief period of observation (3-6 hours), a repeat x-ray to ensure the pneumothorax is not enlarging, and close outpatient follow-up. If the patient is symptomatic, treatment options include aspiration, insertion of a pigtail catheter, or insertion of a small-bore standard chest tube. Aspiration is performed in a manner similar to thoracentesis. Pigtail catheters are smaller and more comfortable for patients than even a small chest tube. If a catheter is placed with a Heimlich or other one-way valve and the patient is reliable, discharge with close outpatient follow-up is a reasonable plan.
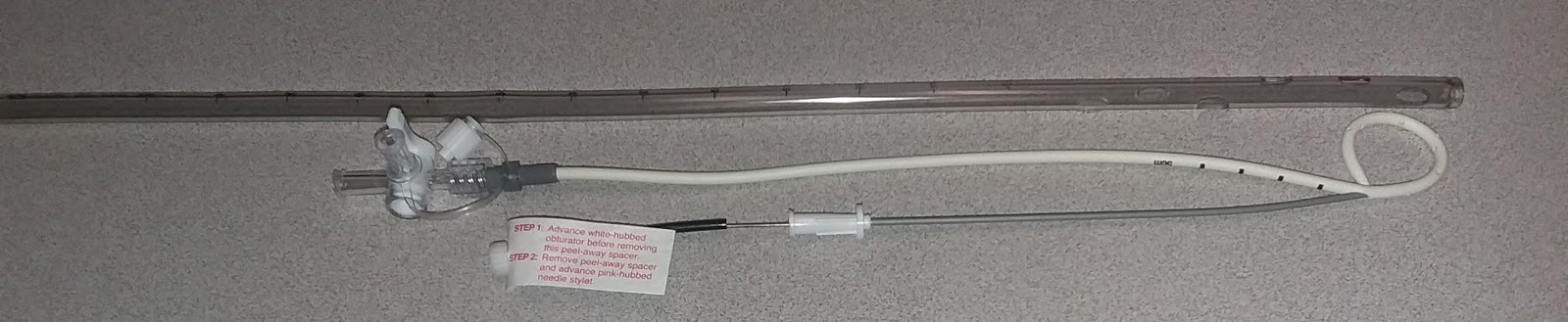
Figure 6 –A commercial pigtail catheter, compared to a 24Fr chest tube.
Image used by permission of Doug Franzen, MD
A larger primary spontaneous pneumothorax (pleural line >2-3cm from the chest wall) or any secondary pneumothorax will usually require admission in addition to drainage via catheter or chest tube. Research has shown that patients with secondary spontaneous pneumothorax frequently fail conservative management such as observation or simple aspiration. Caution is advised before draining a secondary pneumothorax, to ensure it truly is a pneumothorax and not a large bleb. Patients with a recurrent pneumothoraces may require a more aggressive management plan such as thoracoscopy and pleurodesis.
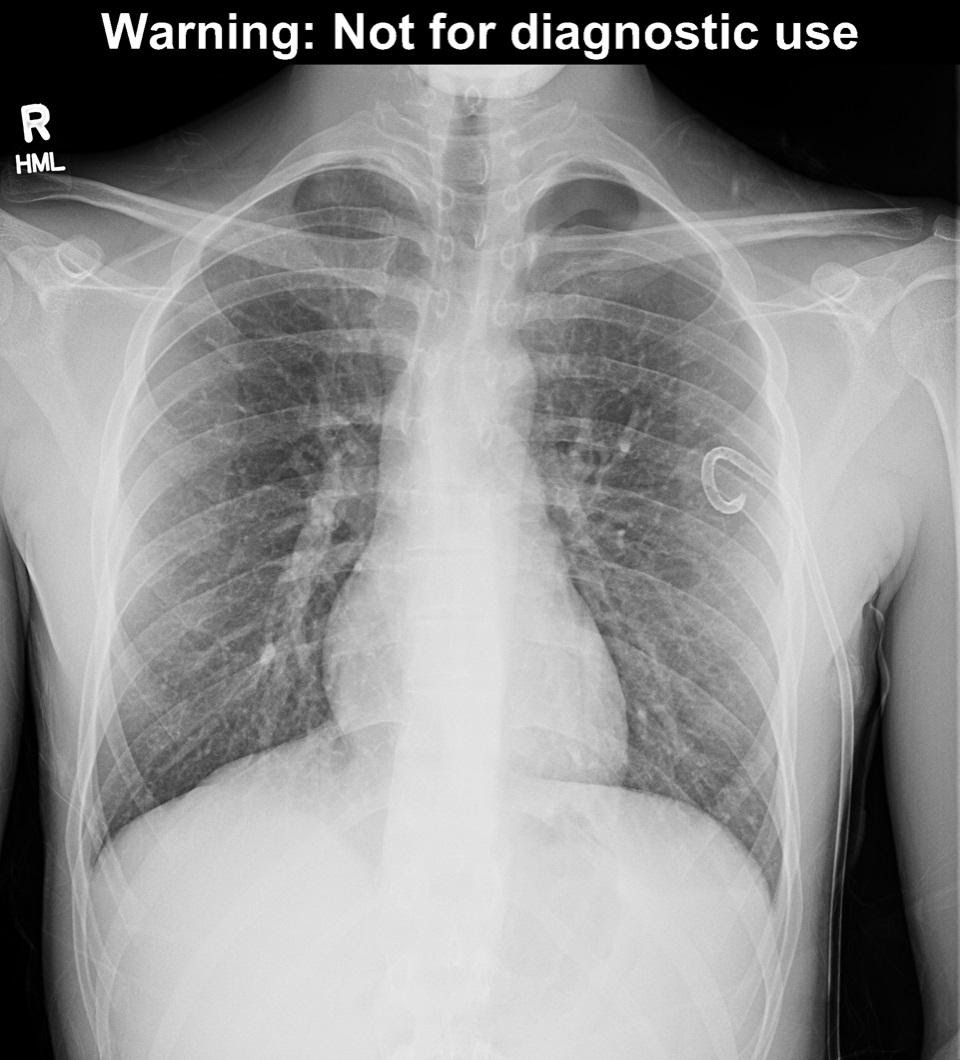
Figure 7 – Pigtail catheter placement. Note that the pneumothorax is still present. This patient (the same patient from Figure 1) ultimately required surgical intervention to treat his pneumothorax. Image used with permission of Joel Gross, MD.
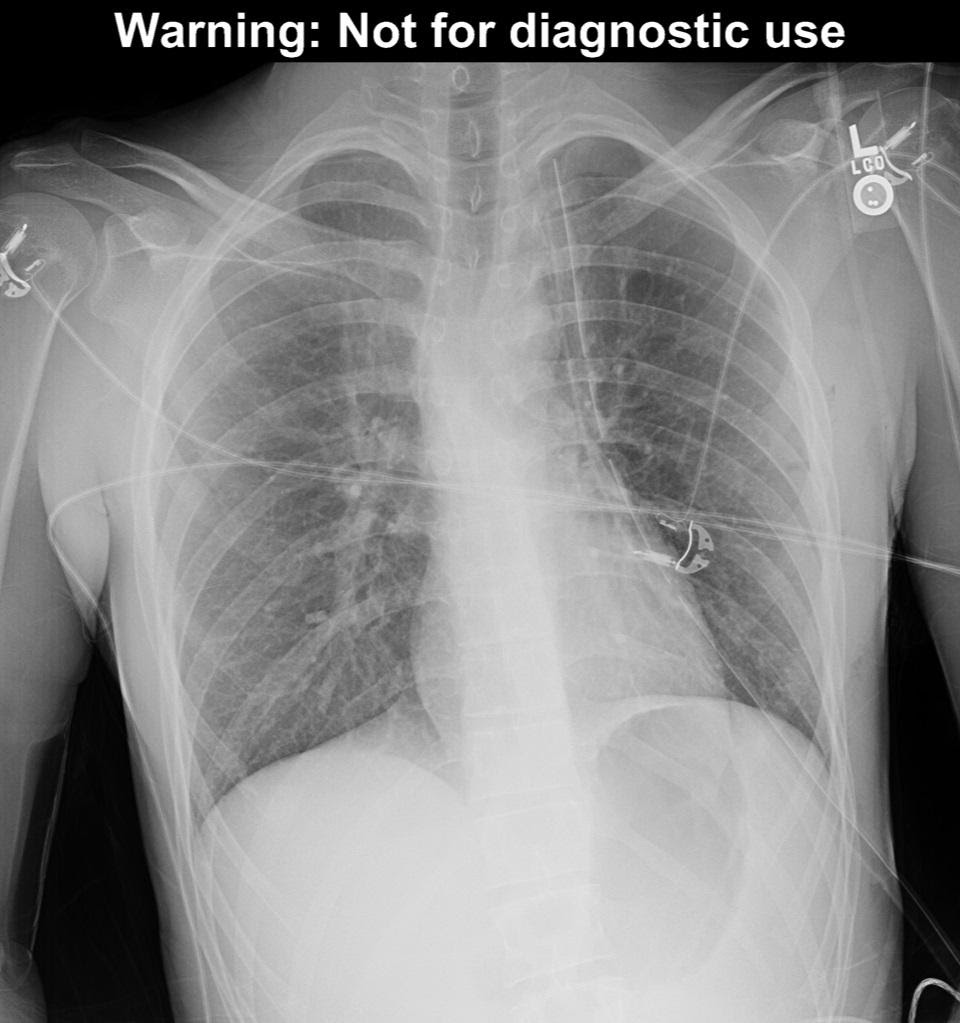
Figure 8 – The patient from figure 7, with a chest tube in place. The pneumothorax has resolved. Image used with permission of Joel Gross, MD.
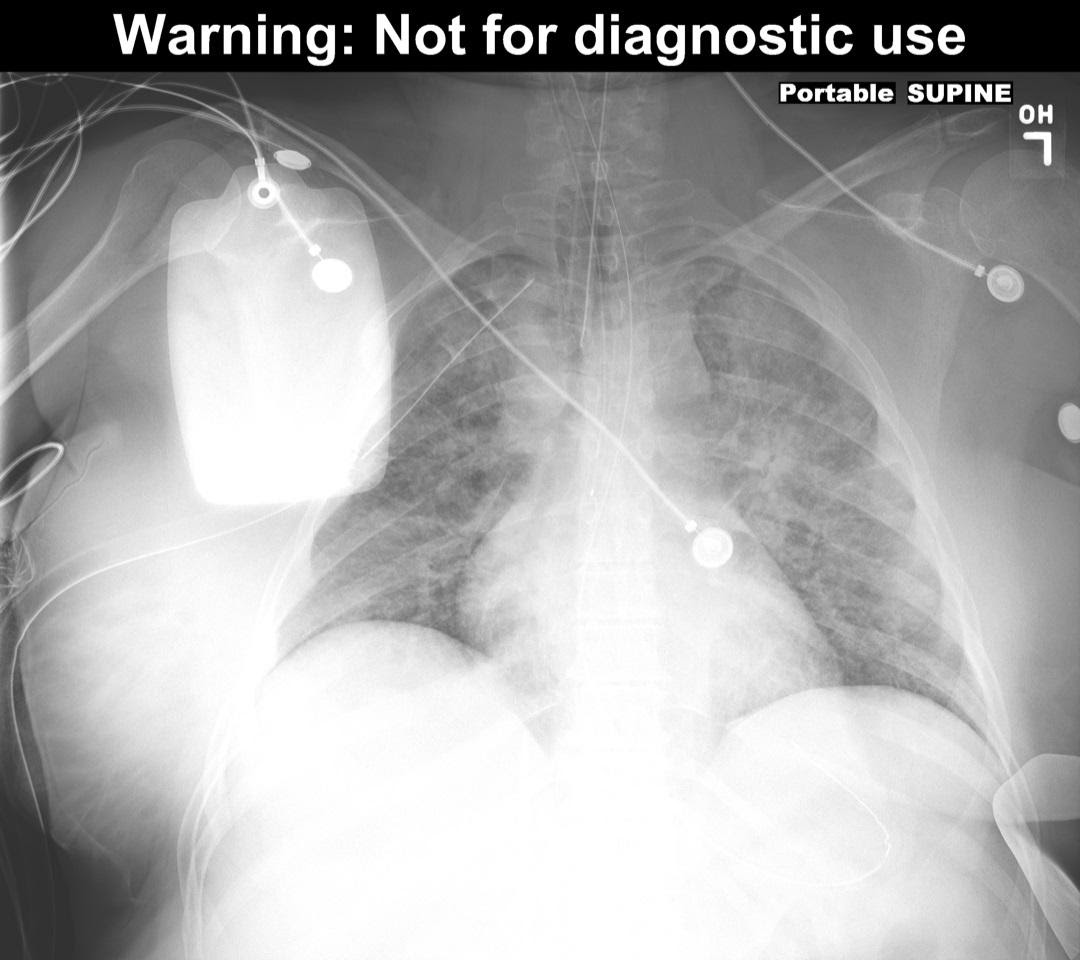
Figure 9 – Resolution of deep sulcus sign after chest tube placement. (This is the patient from Figure 2). Image used with permission of Joel Gross, MD.
Pearls and Pitfalls
- Pneumothorax should be considered in all patients with chest pain and/or shortness of breath
- The classic findings of a tension pneumothorax are late findings.
- Do not wait for a chest x-ray to decompress a suspected tension pneumothorax
- Remember that pneumothorax can be a cause of decompensation in intubated patients, especially after CPR
- Ultrasound is more sensitive than chest x-ray in diagnosing pneumothorax, especially in a supine patient.
Case Study
A targeted history decreased your concern for most of the items on your differential, other than pneumothorax. Physical exam was notable for decreased breath sounds and hyperresonance to percussion of the left chest. There was no JVD and the trachea was midline. Because the patient was stable, a bedside ultrasound was performed, which demonstrated absence of pleural sliding or comet tails on the left. M-mode ultrasound showed a “bar code” appearance on the left. An upright chest x-ray showed a moderate pneumothorax, with a pleural line approximately 3cm from the chest wall. The patient did not have insurance or a primary care provider. Due to all of these factors, a pigtail catheter was placed, and the patient was admitted for observation with resultant improvement in his symptoms. Repeat x-ray after pigtail placement showed marked improvement in the pneumothorax.
References
- Alrajab S, Youssef AM, Akkus NI, Caldito G. Pleural ultrasonography versus chest radiography for the diagnosis of pneumothorax: review of the literature and meta-analysis. Crit Care. 2013 Sep 23;17(5):R208
- Carr JJ, Reed JC, Choplin RH, et al. Plain and computed radiography for detecting experimentally induced pneumothorax in cadavers: implications for detection in patients. Radiology 1992; 183:193.
- Kosowsky J and Kimberly H. Pleural Disease. In: Walls R, Hockberger R, Gausche-Hill M, editors. Rosen's Emergency Medicine: Concepts and Clinical Practice. 9th Ed. Philadelphia: Elsevier. 2018. pp 881-889.
- Nicks BA, Manthey D. Pneumothorax. In: Tintinalli JE, Stapczynski J, Ma O, Yealy DM, Meckler GD, Cline DM. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e New York, NY: McGraw-Hill; 2016. http://accessmedicine.mhmedical.com/content.aspx?bookid=1658§ionid=109429615. Accessed April 9, 2019
- Wong A, Galiabovitch E, Bhagwat K. Management of primary spontaneous pneumothorax: a review. ANZ J Surg. 2019 Apr;89(4):303-308.
