Vascular Access
Author Credentials
Author: Andrew Kendle, MD, The Ohio State University; Christopher E. San Miguel, MD, The Ohio State University
Editor: Carl Preiksaitis, MD/ Stanford University (2022 Revision)
Section Editor: William Alley, MD, Wake Forest School of Medicine
Update: 2023
Case Study
A 72-year-old male patient with a history of end stage renal disease on hemodialysis (via a right internal jugular tunneled catheter) presents with a chief complaint of fever. You immediately head to the room when you note the patient’s critical vital sign abnormalities - he is febrile to 38.5℃, hypotensive to 74/30 mm Hg, and tachycardic to 130 bpm. Unfortunately, initial attempts at peripheral intravenous access are unsuccessful and you are unable to obtain labs or give fluids. The nurse looks over to you and asks, “We need to get some vascular access doc!”
Objectives
By the end of this module, the student will be able to:
Describe the differences among and between various forms of peripheral and central vascular access
Appropriately select a vascular access method based on the indications and contraindications
Introduction
Peripheral intravenous access is among the most common procedures in medicine–with varied estimates of frequency in the range of 150-300 million per year (ref. 1). These and other forms of vascular access are critical for blood sampling, medication administration, and resuscitation with fluid or blood.
Global risks of vascular access include:
bleeding
infection
damage to surrounding structures
The degree of risk for each complication changes based on the type of vascular access placed. In general, any kind of vascular access is contraindicated in extremities with an arteriovenous fistula, prior lymph node dissection, or overlying infection. Beyond this, there is much to know about each type of access. Knowledge of when and how to use which type of vascular access is necessary to safely care for patients.
Nomenclature
When discussing vascular access, perhaps the most distinguishing factor is whether the access is described as peripheral or central. Any catheter which reaches a great venous vessel is considered central. These vessels include the internal jugular, subclavian, and brachiocephalic veins from the neck and upper extremities, the common femoral and iliac veins from the lower extremities, and the superior and inferior vena cava. All other vascular access is considered peripheral. The importance of this distinction is discussed in detail in the following sections.
Venous access catheters are also commonly described by their size. The most important physics factor in the flow rate of vascular access is the diameter, followed distantly by the length of the catheter. In general, the larger the diameter and the shorter the length of the catheter the faster the flow rate according to Poiseuille’s law (Ref 2). The length is typically described in inches; however, the most common measurements you will hear in the hospital refer to the diameter of the lumen of the catheter, as this is the most significant factor in terms of peak flow rate. Somewhat confusingly, smaller peripheral intravenous catheters (PIVs) use a gauge (G) system and larger catheters use a French gauge (Fr) system to classify their respective diameters.
The history of the G system is complicated and beyond the scope of the article, but clinicians should know that the relationship between G and catheter diameter is indirect and non-linear. For example, a 12G PIV has a larger diameter than a 24G PIV, but it is not twice the size of the smaller catheter. In contrast, the Fr system is both directly and linearly related to the diameter, as each Fr is measured at ⅓ of a millimeter. A 12 Fr catheter is therefore 4 mm in diameter, and a 6 Fr catheter is 2 mm in diameter. Finally, to add an additional layer of complexity, some venous access devices are described using both systems. Most triple-lumen central venous catheters are 7 Fr in total diameter, but within the device are 3 lumens with individual measurements of 16G, 18G, and 18G. Because these lines are longer than PIVs, the flow rates are actually slower through these lumens than PIVs of the same diameter. Table 1 lists flow rates for various intravenous access devices (Ref 2, 3).
Flow Rates for Various Intravenous Access Devices | ||
Line | Maximum Flow Rate with pressure | Time to infuse 1 Liter |
8.5 Fr rapid infusion catheter | 857 mL/min | 70 seconds |
14G PIV | 584 mL/min | 103 seconds |
16G PIV | 412 mL/min | 146 seconds |
18G PIV | 205 mL/min | 5 minutes |
20G PIV | 144 mL/min | 7 minutes |
16G Triple Lumen | 116 mL/min | 8.5 minutes |
18G Triple Lumen | 79 mL/min | 12.5 minutes |
Table 1: Flow Rates for Various Intravenous Access Devices.
Access Types
Peripheral Intravenous access
Landmark guided PIV access is first line for the majority of indications. PIVs are generally the fastest and lowest-risk form of access. The most common placement site using landmark guidance is the distal upper extremity (Figure 1).

Figure 1. Peripheral IV in the upper extremity. Image courtesy of Michael Berry. Used under the Creative Commons Attribution 3.0 Unported license. Original image located at: Peripheral venous catheter - Wikipedia.
In patients with difficult access, the external jugular vein (EJ) can be a useful site for IV placement, but insertion in this location often needs to be done by an MD. To be clear, these IVs are not placed blindly. Rather, the operator examines the arm after placing a tourniquet and attempts to identify an enlarged vein “landmark” either by site or by touch. The lower extremity is an option for PIV placement but carries an increased infection risk, and is therefore rarely utilized (Ref. 1).
Peripheral IV access can also be obtained in the proximal upper extremity. Generally, this will require the use of an ultrasound machine (US) to identify the deeper veins of the upper arm. US-guided PIV can also be placed in the distal upper extremity when an adequate vein cannot be identified on physical exam. In order to reach deeper vessels and prevent dislodgement, these catheters have longer lengths than other PIVs. US-Guided PIV placement can be lifesaving for patients who fail landmark-guided PIV placement.
The biggest advantages to PIVs are that they are relatively easy to place, carry very low infection risk, and cause minimal discomfort to the patient. As easily as they are placed, however, they can be lost. They can either move out of the vessel or the walls of the vessel may burst when the “vein blows.” In either case, the PIV can no longer be used. PIVs generally last from hours to days. The increased risk of extravasation as well as direct irritation to smaller vessels is the reason why some medications require central access to be administered. Traditionally this included all vasopressors (such as epinephrine, norepinephrine, and dopamine). However, over the last 5-10 years, numerous studies have shown that peripheral administration of vasopressors is quite safe for up to two days of use (Ref. 4).
The New England Journal of Medicine’s Videos in Clinical Medicine series demonstrates peripheral IV placement:
The following video describes Ultrasound-guided intravenous access placement:
Intraosseous Access

Figure 2. Intraosseous access device. Image courtesy of: Leidel BA, Kirchhoff C, Bogner V, Stegmaier J, Mutschler W, Kanz KG, Braunstein V. Is the intraosseous access route fast and efficacious compared to conventional central venous catheterization in adult patients under resuscitation in the emergency department? A prospective observational pilot study. Patient Saf Surg. 2009 Oct 8;3(1):24. doi: 10.1186/1754-9493-3-24. PMID: 19814822; PMCID: PMC2764565.. Used under the Creative Commons Attribution 2.0 License. Original image: Category:Intraosseous infusion devices - Wikimedia Commons.
Intraosseous (IO) devices (Figure 2, Wikimedia commons EZ-IO drill) offer a rapid, safe option for short term (<24h) vascular access (Ref. 5). This is the only form of vascular access which is faster than a PIV. With the most common placement device, access can be obtained in as little as 20 seconds. This is due to the fact that the target of bone marrow is much larger than a small peripheral vein. IOs are most commonly placed in the proximal tibia or humerus but can also be placed in the distal femur and distal tibia. Whichever site is chosen, IO access requires placement in a normal, healthy bone to minimize the risks of fracture and extravasation which could lead to compartment syndrome.
Contraindications to IO placement include:
Known fracture of the bone
Local orthopedic hardware
Structural bone disorders such as osteogenesis imperfecta
Unique to IOs, is the fact that it is often difficult to use IOs to obtain blood samples. Blood aspirated from an IO can be sent to the lab for analysis but will yield significantly different results than venous samples on a number of typical tests including white blood cell counts, platelet counts, potassium, carbon dioxide, sodium, and calcium levels (Ref. 6). In terms of medication and fluid administration, any drug or blood product that can be given IV can also be given through an IO. This includes vasoactive medications like epinephrine.
The most significant limiting factor for IO use is the associated infection rate. In order to minimize the risk of developing osteomyelitis, IOs should be removed within 24 hours of use. So, while this is the fastest way to gain access, it is also the most short-lived. Patient discomfort is another consideration that often limits the use of an IO. With current insertion devices, the pain with placement is comparable to a PIV. However, the administration of fluid volume can be quite painful as it increases pressure within the bone marrow. Consequently, if an IO is placed in an awake patient, it is recommended to administer lidocaine through the IO prior to the infusion of fluids or other medications.
The New England Journal of Medicine’s Videos in Clinical Medicine series demonstrates placement of IO access in adults:
In children, you can learn to place IO access in the following video:
A good article about establishing IO access is located on Taming The SRU website:
Central Venous Access
Central Venous Catheters (CVCs) are quite varied, from the common multi-lumen CVC to large single bore catheters to special catheters used for long term access. As mentioned above, the commonality between these devices is that they all end in the central venous system. Compared to PIV, the benefits of a CVC include more reliable access, greater longevity, and the ability to administer caustic medications. CVCs also allow for specialized measurements or interventions, such as central venous pressure monitoring, temperature management, or transvenous pacing.
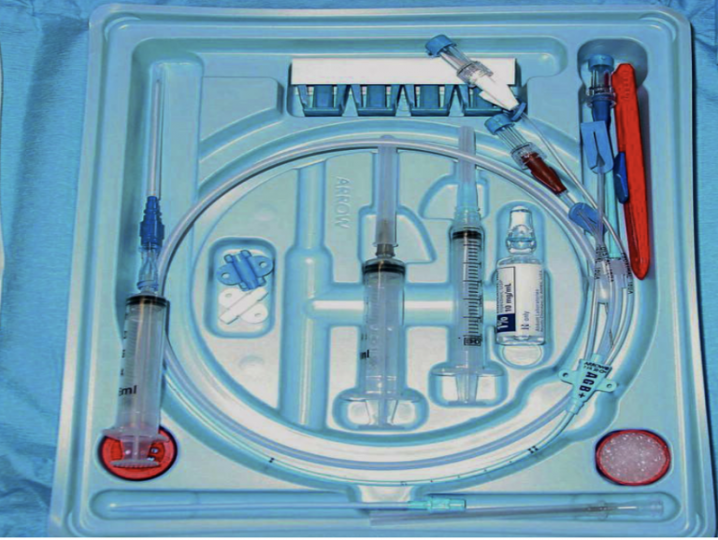
Figure 3. Central line kit for use with the Seldinger technique. Image courtesy of EMDocs. Used under the Creative Commons Attribution 4.0 International License. Original image located at: emDOCs.net – Emergency Medicine EducationUnlocking Common ED Procedures: Never Let Go - A Review of Central Venous Access Placement - emDOCs.net - Emergency Medicine Education.
In the Emergency Department (ED), the most commonly placed CVCs are multiple lumen CVCs (Ref. 7), large bore rapid infusion catheters, and specialized catheters used for temporary hemodialysis access or targeted temperature management. All of these catheters are placed directly into the central venous system via the internal jugular, subclavian, or femoral veins. This is a physician-level procedure that requires sterility and, in most cases, ultrasound guidance. Multiple lumen CVCs are the most useful for patients that require multiple different access points and have unreliable or nonexistent peripheral access. A common scenario might be a septic patient in diabetic ketoacidosis (DKA) who is going to simultaneously require fluid resuscitation, an insulin drip, antibiotics, and electrolyte replacement. Because of its much faster flow rate, a large bore rapid infusion catheter, such as the Cordis or introducer sheath, (Figure 4), is preferred in instances of high-volume resuscitation like a trauma patient in hemorrhagic shock.
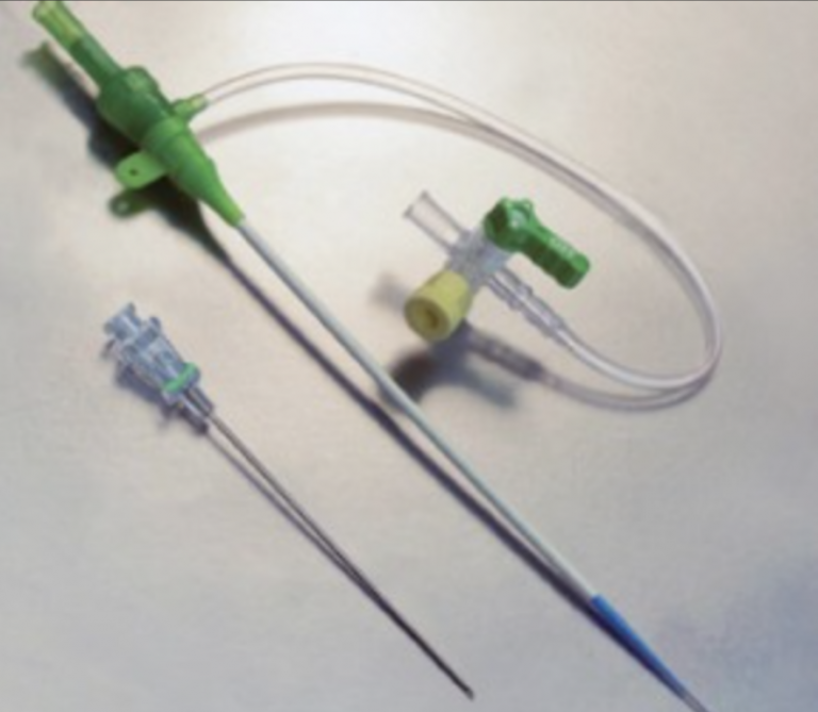
Figure 4. Example of a type of central line catheter- Introducer sheath. Used under the Creative Commons Attribution 4.0 International License. Original image located at: emDOCs.net – Emergency Medicine EducationUnlocking Common ED Procedures: Never Let Go - A Review of Central Venous Access Placement - emDOCs.net - Emergency Medicine Education.
There are numerous considerations when selecting where to place the CVC in the ED, but site selection is largely driven by practicality and potential adverse events during placement. As with any invasive procedure, there are risks of bleeding, infection, and damage to surrounding tissue during the insertion of the CVC. Infection is the major drawback of centrally inserted CVCs. With a rate of 2.5 per 1000 line-days these catheters are second only to IOs in terms of infection rate (Ref. 1) Another common risk to all sites is arterial injury, as all of these central veins run alongside central arteries. Air embolism and retained guidewire can potentially occur at any site, but only IJ and more so subclavian placement carry the additional risk of causing a pneumothorax. In addition, if excessive bleeding occurs, compression of the subclavian vein is challenging due to its anatomic location. Therefore this site is less favorable for patients with increased bleeding risk, such as those with coagulopathy. In terms of practical considerations, if central access is required in a patient undergoing CPR, a femoral site is often chosen as chest compressions make IJ and subclavian placement difficult. A femoral CVC might also be placed if the patient is shortly going to undergo a procedure that will require access to the superior vessels, such as hemodialysis line or pacemaker placement.
The most common indications for non-emergent CVC include the administration of certain vein-damaging medications (caustic electrolytes, vasopressors) and the need for long term access (chemotherapy, dialysis, prolonged IV antibiotics). Specialized function CVCs include dialysis catheters (with ports for dialysate flow) and cooling lines (with a sheath that cool or warm fluid can circulate through). Since centrally inserted CVCs have such high infection rates, patients generally don’t leave the hospital with these in place. Instead, central access is obtained by specialized devices with lower infection rates (Figure 5). For example, tunneled catheters are “tunneled” from a skin insertion site through the subcutaneous tissue into either the IJ or subclavian veins to reach the superior vena. As a result, the catheter exits the skin on the upper chest. These are similar to ports which also tunnel under the skin before reaching a great vein. However, ports do not actually exit the skin, rather skin grows over a small chamber with a silicon top. To use the port, a needle is then inserted through the skin and silicon top and goes directly into the chamber. This allows the access site to be less intrusive in daily life as there is nothing outside of the skin, but accessing the port is a little uncomfortable and requires special training and equipment. Finally, peripherally inserted central catheters (PICC) are used for midterm use. The catheter is inserted in the upper arm but the tip ends up in the SVC. Mid-term IV antibiotic administration is a classic indication for a PICC line.
Table 2. Characteristics of different kinds of vascular access.
The New England Journal of Medicine’s Videos in Clinical Medicine series demonstrates how to establish different kinds of central access:
Central Venous Catheterization
Placement of a Femoral Venous Catheter
Ultrasound Guided Internal Jugular Line placement
Subclavian Catheter placement
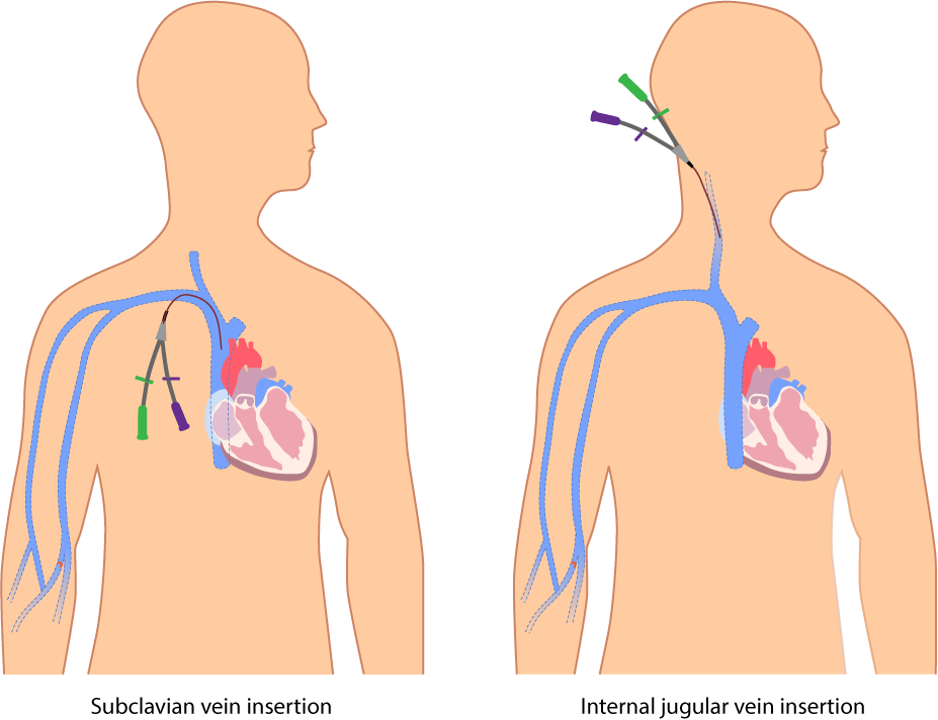
Figure 5. Subclavian and Intrajugular central venous access. Image courtesy of Glynda Rees Doyle and Jodie Anita McCuthcheon. Used under the Creative Commons Attribution 4.0 International License. Original Image located at: central-venous-catheter.png (927×713) (opentextbc.ca).
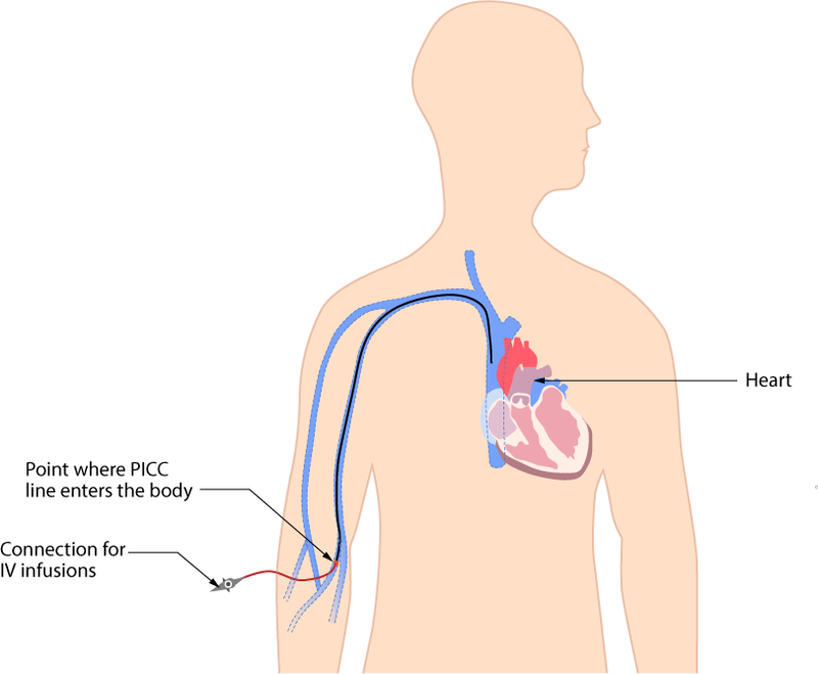
Figure 6. PICC (Peripherally Inserted Central Catheter). Used under the Creative Commons Attribution 4.0 International License. Original Image located at: 8.2 Intravenous Fluid Therapy – Clinical Procedures for Safer Patient Care (opentextbc.ca).
Pearls and Pitfalls
Practice PIV placement and US-guided PIV placement, as these are critical skills that will atrophy
Large bore PIV is usually the best resuscitation method - place two for redundancy and additive flow
Do not delay IO placement if indicated, but also consider the external jugular
Remember your catheter flow rates - do not try to resuscitate with a triple lumen CVC
Be familiar with multiple forms of access, as different patients require different access
Case Study Resolution
Both landmark guided and ultrasound-guided peripheral IV placement fail in this critically ill dialysis patient. You are able to place a single external jugular IV and proximal tibia IO to obtain initial labs and start fluids. You note that his left chest wall hemodialysis catheter appears infected. Because of this, you opt to place a femoral CVC for access to administer multiple medications, calcium chloride, and pressors. You have preserved his right IJ/subclavian for anticipated hemodialysis access. He is admitted to the ICU, where he has his left-sided catheter removed and a new right-sided hemodialysis catheter placed. He recovers from his MRSA bacteremia and eventually has a PICC line placed for ongoing vancomycin infusions.
References
Maki DG, Kluger DM, Crnich CJ. The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc. 2006;81(9):1159-1171. doi:10.4065/81.9.1159. PMID: 16970212.
Reddick AD, Ronald J, Morrison WG. Intravenous fluid resuscitation: was Poiseuille right? Emerg Med J. 2011;28(3):201-2. doi: 10.1136/emj.2009.083485. PMID: 20581377.
Barcelona SL, Vilich F, Coté CJ. A comparison of flow rates and warming capabilities of the Level 1 and Rapid Infusion System with various-size intravenous catheters. Anesth Analg. 2003;97(2):358-363. doi: 10.1213/01.ANE.0000070235.67887.5C. PMID: 12873917.
Cardenas-Garcia J, Schaub KF, Belchikov YG, Narasimhan M, Koenig SJ, Mayo PH. Safety of peripheral intravenous administration of vasoactive medication. J Hosp Med. 2015;10(9):581-585. doi: 10.1002/jhm.2394. PMID: 26014852.
Dornhofer P, Kellar JZ. Intraosseous vascular access. In: StatPearls. StatPearls Publishing; 2022. PMID: 32119260.
Miller LJ, Philbeck TE, Montez D, Spadaccini CJ. A new study of intraosseous blood for laboratory analysis. Arch Pathol Lab Med. 2010;134(9):1253-1260. doi: 10.5858/2009-0381-OA.1. PMID: 20807043.
DeVivo A. Unlocking common ED procedures: never let go - a review of central venous access placement. emDOCs. http://www.emdocs.net/unlocking-common-ed-procedures-never-let-go-a-review-of-central-venous-access-placement/. Published February 13, 2020. Accessed January 2, 2023.
