Trauma
Objectives
Upon finishing this module, the student will be able to:
- Understand the physiologic differences between pediatric and adult trauma victims.
- Perform a rapid primary survey using ABCDEF.
- Discuss the secondary survey for the pediatric trauma patient with special attention to head, cervical spine, chest, and abdominal trauma.
Contributors
Update Authors: Zack Dunn, DO; and Jeremiah Smith, MD.
Original Authors: Jeremiah Smith, MD; and Sean Fox, MD.
Update Editor: Navdeep Sekhon, MD.
Last Updated: May 2024
Introduction
In the United States, accidental injuries are consistently the leading cause of death each year in children over the age of one. Each year, approximately 8,000 children and adolescents die from unintentional injuries. The approach to the pediatric trauma patient is a bit different than the approach to trauma in the adult patient due to:
- The different physiology of the pediatric patient.
- The different injury patterns and anatomy of the pediatric patient.
- The different evaluation pathways and risk stratification rules.
Emergency physicians must be comfortable in pediatric trauma stabilization to prevent additional morbidity and mortality in the pediatric population.
A 13-year-old male presents via EMS after a dirt-bike collision. The patient was riding his dirt bike in the woods and flipped over the handlebars after crashing into a large root. He was wearing a helmet. He denies any head injury, nausea or vomiting, loss of consciousness, or changes in mentation. His vital signs are BP 90/58, P 120, R 22, and T 36.9°C (98.4°F); SpO2 is 95% on room air.
He arrives with his cervical spine immobilized. On initial evaluation, the patient is talking and maintaining his airway, his breath sounds are clear to auscultation bilaterally, and he has strong pulses in all extremities. He has a GCS score of 15, superficial abrasions to his lower extremities and forearms, and bruising across his upper abdomen. He has tenderness to palpation in his epigastric region with guarding and pain with any movement. His pain is reported as a ten out of ten. The patient’s blood pressure improves with 20 mL/kg of intravenous crystalloid fluids.
How Should You Initially Evaluate a Child who has had a Traumatic Injury?
- Always start with the primary survey.
- Address any problems identified on the primary survey before moving on with your evaluation.
- Log roll the patient and get them off the backboard when able.
- Perform the secondary survey with FAST exam and x-rays.
- If the patient begins to deteriorate, reassess the patient and restart your evaluation with the ABCs.
- Remember this is likely a very terrified child and this can alter your exam. When able, always include family members to help calm and comfort the child.
Primary Survey
The initial assessment and survey is not significantly different from adults. However, children have a unique physiologic response to trauma, creating challenges in their management. Start with the primary survey as with adult patients. You will evaluate and address problems with one system before moving to the next. In reality, this is often done simultaneously. Always have a consistent, systematic approach in the evaluation of a patient with traumatic injuries like Advanced Trauma Life Support (ATLS).
- A - Airway (with cervical spine protection)
- B - Breathing
- C - Circulation
- D - Disability (neurologic assessment)
- E - Environment/exposure
- F - Family
Airway
The first priority is to determine if the airway is open and patent. Is the child speaking? If they are nonverbal, are they crying? This is a frightening experience for most young children, so be wary of the silent child. Pediatric airways have similar complications secondary to trauma compared to adult airways that may lead to loss of a patent airway and a difficult intubation. These include:
- Foreign body in the airway.
- Facial fractures and bleeding.
- Tracheal injuries.
- Expanding hematomas.
- Depressed level of consciousness and inability to protect airway.
It is important to note that sometimes the airway of the pediatric patient is more anterior than those of adults and the tongue may be larger in proportion. If a child does not have a patent airway or is at risk of losing their airway, act quickly.
- Always maintain C-spine immobilization.
- Use simple airway maneuvers (jaw thrust, nasopharyngeal airway, oropharyngeal airway) or bag-valve mask (BVM) ventilations if these seem ineffective.
- Rapid sequence intubation (RSI) may be required to stabilize a lost airway or protect a tenuous one.
- Children with significant airway edema, abnormal anatomy, foreign body, or significant maxillofacial injuries may require cricothyroidotomy (surgical or needle).
- With infants and younger children, needle cricothyroidotomy is preferred over surgical cricothyroidotomy due to more pronounced differences in airway anatomy. Needle cricothyrotomy and percutaneous translaryngeal ventilation can be achieved by administering short bursts of oxygen delivery through a small bore catheter followed by a passive exhalation phase (jet ventilation).

Figure: Needle cricothyrotomy. Image courtesy of EMCurious, used under the Creative Commons Attribution 4.0 International License. Original image located here.
The pediatric airway has both anatomic and physiologic differences that set it apart from an adult airway.
- Prominent occiput - forces flexion of the neck in the supine position, potentially obstructing the airway and adding difficulty to the intubation.
- Larger tongue.
- Larger adenoid tissue.
- Floppy, omega-shaped epiglottis.
- Larynx is more cephalad and anterior.
- Cricoid ring, not the vocal cords, is the narrowest portion of the airway.
- Shorter tracheal length.
Breathing
Once you have evaluated and stablized the airway, it's time to evaluate the patient's breathing. As with adults, you will need to look, feel, and listen to the chest in children.
- Inspect: Look for tracheal deviation, accessory muscle use, chest wall injury, and paradoxical breathing (chest wall moves inward with inspiration and outward with expiration).
- Palpate: Feel for crepitus and point tenderness, paradoxical movements with observed paradoxical breathing, or percuss for hyper-resonance or dullness.
- Auscultate: Listen for signs of upper airway obstruction (stridor), signs of pneumothorax (absent breath sounds), or hemothorax (diminished breath sounds). In small children, you can often hear lung sounds from the adjacent lung even if there is a pneumothorax in the lung that is auscultated.
If a child has a patent airway but your evaluation reveals poor breathing, ventilating the child is your next priority.
- BVM ventilation is a temporizing method to ventilate a child, and is one of the most important life-saving skills you need to learn and master.
- A child can be BVM-ventilated until an advanced airway can be placed.
- Select a properly sized bag with a pop-off valve to reduce barotrauma.
- Each breath should be just enough to make the chest rise, avoiding excessive pressure which can cause an iatrogenic pneumothorax.
- An oral airway can greatly assist ventilation in children with macroglossia or any other upper airway obstruction.
Pediatric-Specific Considerations When Evaluating Breathing in a Traumatic Injury
- Children have increased vagal tone and a tendency to become bradycardic with laryngoscope blade manipulation.
- Children have a lower respiratory reserve.
- Children have a higher metabolic demand, and a lower functional residual capacity leads to quicker onset of hypoxia with apnea (shorter apnea time).
- Children fatigue easily because of their compliant chest wall aids less in breathing and they rely more on the diaphragm.
- Hyperextension or hyperflexion of the neck while positioning may lead to airway obstruction.
The respiratory rate is age-dependent. A rate of 15 may be fine for a 12-year-old but would not be for a six-month-old.
- Newborn: 40-60 breaths/minute.
- 6 months: 30-60 breaths/minute.
- 1 year old: 20-40 breaths/minute.
- 2 year old: 20-40 breaths/minute.
- 4 year old: 20-34 breaths/minute.
- 6-14 year old: 18-30 breaths/minute.
- >14 year old: 12-16 breaths/minute.
Children also have anatomic differences in their ribcage to consider in pediatric blunt trauma:
- Higher compliance.
- Less propensity to fracture ribs and release the force from the trauma.
- Increased transmission of blunt force to the underlying lung parenchyma.
- Increased incidence of pulmonary contusion vs rib fracture and subsequent pneumothorax/hemothorax (See the SAEM M4 Curriculum's "Approach to Trauma" article for an overview of pneumothorax and hemothorax).
- Fewer external signs of trauma.
Circulation
Children have a remarkable ability to maintain their blood pressure even with significant volume loss (25-30% blood volume loss). Since children compensate so well (compensated shock), blood pressure is not as accurate a reflection of circulatory status as it is in adults. To assess for circulatory status, it is important to check:
- Feel for central and peripheral pulses (tachycardia is common).
- Skin color.
- Capillary refill.
- Though it is less helpful during the initial survey, urine output is one of your best indicators of volume status (>1-2mL/kg/h).
Pediatrics covers a wide range of ages and it is important to know or have a resource available that lists normal heart rate and blood pressure values for a given age. A good rule to remember is that the 50th percentile systolic blood pressure is 90 + (2 x age in years) up to ten years old and then it is 110 mmHg, similar to an adult.
Heart Rate and Blood Pressure by Age
| Age | Heart Rate (beats per minute) | Blood Pressure (mmHg) |
| Newborn | 140-160 | 40-70/20-45 |
| 6 months | 120-160 | 74-100/50-70 |
| 1 year old | 100-140 | 74-100/50-70 |
| 2 year old | 90-140 | 80-112/50-80 |
| 4 year old | 80-110 | 84-112/54-80 |
| 6-14 year old | 75-100 | 84-120/54-80 |
| >14 year old | 60-90 | 94-141/62-88 |
Progression to decompensated shock will quickly lead to complete cardiopulmonary failure. Shock is a reflection that end organs are inadequately perfused and oxygenated. It must be identified and treated quickly.
- Hemorrhagic shock is the most common etiology of shock in the setting of a traumatic injury.
- Intravenous access is essential: obtain two large bore intravenous catheters in the trauma patient with evidence of shock.
- If peripheral intravenous access is difficult or taking too much time, rapid placement of an intraosseous (IO) needle can be life-saving.
- Initially give 20mL/kg of isotonic fluids (typically normal saline).
- Fluids should be given rapidly using either a pressure bag or via the three-way stopcock "pull-push" method.
- If a child has not had an adequate response after two boluses, consider giving 10mL/kg of packed red blood cells.
- Continue to fluid resuscitate the child during the ongoing evaluation and treatment of specific injuries.

Figure: Intraosseous access device. Image courtesy of reference 11. Used under the Creative Commons Attribution 2.0 License. Original image located here.
Disability
Similar to adults, the disability examinations should rapidly assess a child for neurologic deficits. The American Heart Association (AHA) Pediatric Advanced Life Support (PALS) program recommends the use of the mnemonic AVPU in children as well.
- Alert: Fully alert.
- Voice: Responds to voice.
- Pain: Responds to pain.
- Unresponsive: Is completely unresponsive.
This can quickly be assessed while doing a gross motor/sensory examination. The simplest way is to ask an appropriately aged child to wiggle their fingers or toes and see how they respond. Infants and younger children require more direct observation and interaction but can still be quickly assessed in the trauma bay. This does not replace the need for a thorough neurologic exam and will be performed during the secondary survey. A quick pupillary examination is typically done at this time as well. You are assessing for size, symmetry, and reactivity. Unresponsive and dilated pupils are worrisome for uncal herniation and emergent intervention will be needed.
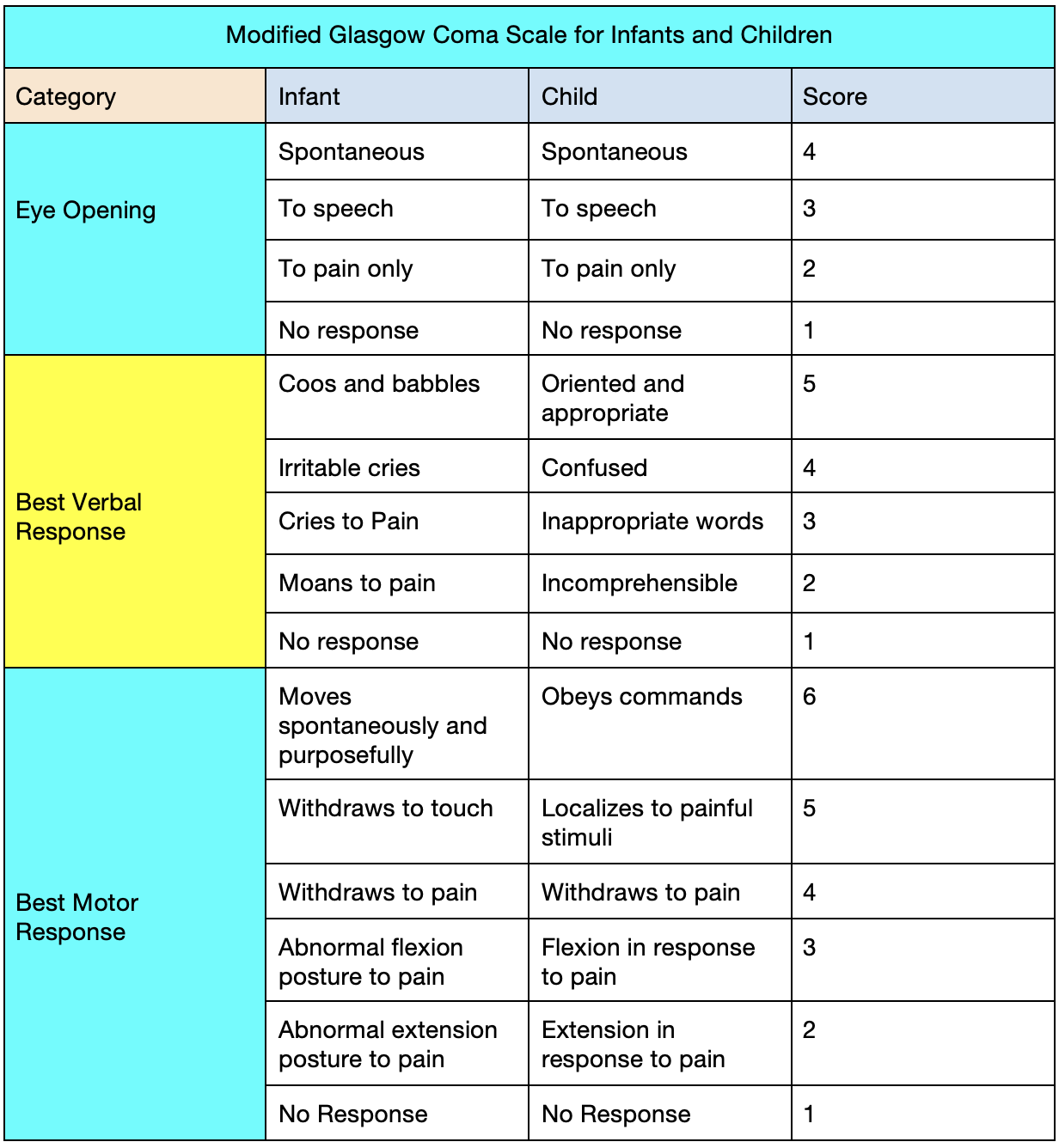
PALS also recommends the use of the validated Modified Glasgow Coma Scale for Infants and Children to quickly evaluate mental status. The best possible score is 15 and the lowest is 3.
A rapid bedside glucose should be checked as well. Children are prone to have hypoglycemia due to smaller glycogen stores as well as a higher metabolic demand. Hypoglycemia can have a profound effect on a child's mental status and will require emergent interventions (typically a bolus of intravenous dextrose).
Finally, you should logroll the child while maintaining cervical spine immobilization and palpate the spine for tenderness and step-offs. You should remove the backboard at this time as well. Logrolling is a carefully orchestrated maneuver intended to maintain inline cervical spine immobilization.
Environment/Exposure
All children must be fully undressed and examined thoroughly for hidden (occult) injuries. The metabolic needs of children are increased by hypothermia and maintenance of normothermia is paramount. After exposure, it is important to maintain normothermia. This can be accomplished with the use of warm blankets, warmed intravenous fluids, and a warm ambient temperature in the trauma bay.
Family
The ED trauma bay can be loud and frightening for young children, impacting the assessment of a child. Allowing family members to comfort and guide the child during the evaluation can provide a more accurate evaluation. A child life specialist can be invaluable if a family member cannot be present.
It has been shown that family presence during a resuscitation is beneficial to the grieving process as well. However, one specific person (child life, chaplain, social worker) should be the point person who can answer all of their questions during this experience.
Secondary Survey
The secondary survey is a head to toe examination that only begins once all problems identified on the primary survey have been addressed and the child is stable.
History
This is when you should obtain a focused history if the child is able to give it or if there is a caregiver present. This is best obtained using the AMPLE mnemonic.
- A: Allergies
- M: Medications
- P: Past medical history
- L: Last meal
- E: Environments and events associated with injury
Physical Exam
Head Trauma
Head injury is the leading cause of death and disability in children. The relative size of a child's head compared to their trunk is larger, which places more torque on the cervical spine, making it more prone to injury. Children are also more susceptible to shear injury because their brains are less myelinated. It is also important to consider non-accidental trauma (NAT) when evaluating a child with head trauma. As a result, the head exam must be thorough and systematic in children.
- Inspect and palpate the skull for step-offs or lacerations.
- Battle's sign (bruising behind the ear), raccoon eyes (periorbital bruising without swelling), and/or hemotympanum (blood behind the eardrum) are worrisome for a basilar skull fracture.
- Scalp hematomas, particularly non-frontal, are worrisome.
- Feel for the anterior fontanelle in a child under one year old.
- An age-appropriate neurologic examination to assess motor and sensory function as well as cranial nerves (a caregiver may notice a subtle abnormality).
- Attempt to limit radiation and unnecessary head CT scans by following the PECARN head injury guidelines.
- The dental exam can easily be overlooked but should be performed, especially looking for injuries that may damage underlying permanent teeth (e.g. impacted tooth).
Neck and Spine Trauma
Cervical spine injuries in children vary from adults due to anatomic differences: larger head size with greater flexion and extension, weaker paraspinal musculature, increased spinal ligament laxity, infant spinal column can lengthen without rupture, immature vertebral joints, and lack of uncinate processes until about ten years of age. Always assume a child has had a C-spine injury until proven otherwise.
- Most patients will arrive to the ED with pre-hospital C-spine immobilization.
- Maintain immobilization until an injury has been ruled out.
- If a child is too small for a cervical collar, sandbags on either side of their head and tape are an alternative.
- While maintaining C-spine immobilization with a second provider, palpate for midline deformities or tenderness along the C-spine.
- Thorough motor and sensory examination (isolated sensory complaints more common).
- Many children are asymptomatic or too uncooperative to provide an adequate examination (use family and child life specialist liberally).
- The typical C-spine decision rules (NEXUS and Canadian) must be used with caution becuase children were under-represented in their study populations.
Chest Trauma
Children have thoracic, anatomic, and physiologic differences from adults that affect injury patterns.
- Compliant chest wall causes fewer rib fractures.
- Compliance can mask underlying injuries and minimize extenral signs of trauma.
- Though increased compliance leads to fewer rib fractures, it also leads to increased pulmonary contusion.
- Mediastinum is more mobile.
The physical exam evaluating the chest is similar in children compared to adults.
- Inspection: Nasal flaring, chest wall injuries, bruising, seat belt sign (shoulder belt), paradoxical chest wall movement.
- Palpation: Crepitus and/or tenderness.
- Auscultation: Muffled heart sounds, abnormal lung sounds (absent, muffled); caution must be used in interpreting breath sounds in a noisy trauma room.
Isolated thoracic injury is uncommon in children. It is more likely to result with a significant injury causing concomitant injuries. Children will have injuries similar to adults. Common pediatric trauma injuries of the chest include:
- Pneumothorax
- Hemothorax
- Pumonary contusion: Responsible for ~10% of all pediatric trauma admissions. Mild to severe hypoxia depending on the extent of contused lung. Always be vigilant because it can worsen over time as contusion evolves. Chest x-ray findings may lag behind injury, but if abnormal represents a significant injury.
- Flail chest: Results from two or more fractures in contiguous ribs (paradoxical chest movement).
- Rib fractures
- Traumatic asphyxiation: This occurs due to increased compliance of the pediatric chest wall and occurs after direct compression of the chest and deep inspiration against a closed glottis with a crush injury. This increases pressure in the superior and inferior vena cava and leads to facial/neck hemorrhage, cyanosis, and facial swelling. Treat by addressing associated injuries and elevating the head of the bed.
- Commotio cordis: Almost solely a pediatric traumatic injury. This is a combination of direct anterior chest injury leading to ventricular fibrillation and sudden cardiac death. Treatment consists of rapid recognition and use of an automated external defibrillator by bystanders or first responders.
Abdominal Trauma
Children have specific anatomic differences that protect them from some injuries but place them at greater risk for others. These differences include:
- Larger solid organs.
- Less subcutaneous fat.
- Less protective abdominal wall musculature.
- Larger kidneys.
- Flexible ribcage, allowing for excursion of the chest wall and abdominal organ compression.
The abdominal exam for children consists of:
- Inspection: Completely undress children to assess for evidence of trauma; bruising (seat belt sign, periumbilical, flank), or tire tracks may be seen.
- Auscultation: Hypoactive bowel sounds.
- Palpation: Point tenderness, rebound, guarding.
- Percussion: Diffuse dullness is a sign of peritoneal injury.
Focused Assessment Sonography in Trauma (FAST) is a quick and non-invasive ultrasonographic evaluation of the abdomen looking for free fluid. Areas looked at in the FAST exam are Morrison's Pouch (hepato-renal), perisplenic (spleno-renal), bladder, and subxiphoid cardiac view. A positive FAST indicates free fluid and should prompt further evaluation. If the patient is unstable, they should go directly to the operating room (OR), otherwise an abdominal CT with intravenous contrast should be obtained. A negative FAST does not rule out serious intra-abdominal injury and further evaluation may still be warranted. For more information, review the CDEM M3 Curriculum FAST Exam chapter.
Pelvic Trauma
Pelvic injuries are uncommon in children, but they should still be inspected and palpated for signs of pain or pelvic instability. If there is concern, pelvic films should be ordered. If there is concern for instability and a pelvic fracture, compression with a wrapped sheet or a pelvic binder should be placed.
Genital, Perineal, and Rectal Trauma
Any signs of genital hematomas, blood at the urethral meatus, or lacerations should be evaluated further. If there is concern for blood, a rectal exam should be performed. Often, visualized rectal tone (anal wink) is sufficient unless neurologic injury (spinal shock) is a concern and then a digital rectal exam should be performed.
Musculoskeletal Trauma
A thorough extremity exam is always needed. Evaluate the neurovascular status. Patients with a gross deformity or point tenderness will need x-rays to evaluate for fracture. Splint deformed extremities to help prevent further injury and alleviate pain.
The differential diagnosis for a child with a traumatic injury can be large. Remember that children have unique anatomy and physiology. Though you perform a similar evaluation that you use with every adult, their specific needs and injury patterns may be different.
The most life-threatening diagnoses that will need emergent intervention include:
- Traumatic brain injury with increased ICP and impending herniation.
- Airway obstruction.
- Respiratory failure.
- Tension pneumothorax.
- Massive hemothorax.
- Large pulmonary contusion.
- Commotio Cordis.
- Blunt abdominal trauma with active hemmorhage.
Laboratory Studies
- EDs commonly have "trauma panels" to assist in the evaluation of pediatric trauma patients.
- Laboratory studies may include complete blood count (CBC), electrolytes (BMP or CMP), coagulation studies (PT/INR and PTT), type and screen, lipase, urinalysis, blood gas, and serum lactate.
- Studies have shown that routine trauma panels do not have much utility when broadly applied in pediatric trauma evaluation, and clinicians should order laboratory studies as clinically appropriate.
Radiographs
- Plain film radiographs are quick and portable means of imaging.
- Chest radiographs can be helpful in assessing for pneumothorax, hemothorax, and rib fractures.
- Extremity radiographs are mainly utilized to evaluate for bony structure abnormalities or fractures.
- Not ideal for identifying soft tissue injuries, but may identify radiopaque foreign bodies.
Computed Tomography (CT)
- CT imaging is a valuable modality of imaging for timely evaluation of injuries to the head, face, neck, chest, abdomen, and pelvis.
- CT scans cannot be done portably and require patients to be stable enough for transport to and from the CT scanner.
Magnetic Resonance Imaging (MRI)
- Generally, MRI imaging cannot be obtained as quickly as CT scans or plain film radiographs.
- MRI imaging can be helpful in the evaluation of the spinal cord, brain, and soft tissues.
- In younger patients or noncompliant patients, sedation may be needed to obtain quality images.
- Be intentional in having family involved and present at the bedside. Physicians may be hesitant to involve families for fear that resuscitation may be delayed or that they will complicate the course, but families can be useful in providing comfort to the pediatric patient. A staff member should be designated as the point of contact for the family.
- As pediatric patients are more prone to acute decompensation from hypoxia, frequent evaluations of the airway is important. Have a low threshold for establishing a secure airway with any sort of decline in mental status.
- The appropriate size for a cuffed endotracheal can be estimated using the formula: size (mm) = (age in years/4) +3.5. After placement, the endotracheal tube depth at the teeth should be three times the tube size.
- Do not assume that persistent and sustained tachycardia is due to anxiety or pain. Tachycardia may be the first sign that a patient is on the verge of decompensation. Hypotension is a very late sign of hemodynamic compromise in the pediatric patient.
- Child abuse or non-accidental trauma may present as a pediatric trauma patient. Make note of suspicious injury patterns or stories that are inconsistent with the mechanism of injury.
- Although CT scans are a powerful tool in evaluating pediatric trauma patients, they should be used judiciously. For lower mechanism head injuries, the PECARN head imaging rules should be followed closely.
- Management of Pediatric Trauma. American Academy of Pediatrics and Pediatric Othopaedic Society of North America. 2008 Apr.
- Avarello JT, Cantor RM. Pediatric Major Trauma: An Approach to Evaluation and Management. Emerg Med Clin N Am. 2007 Aug.
- Fleming S, et al. Normal Ranges of Heart Rate and Respiratory Rate in Children from Birth to 18 Years of Age: A Systematic Review of Observational Studies. Lancet. 2011.
- Hoffman RJ. Pulmonary Contusion. Fleisher & Ludwig's 5-Minute Pediatric Emergency Medicine Consult. Wolters Kluwer Health/Lippincott Williams & Wilkins. 2012. Print.
- Kenefake M, Swarm M, Walthall J. Nuances in Pediatric Trauma. Emerg Med Clin N Am. 2013 Aug.
- Pediatric Advanced Life Support (PALS). Heart Attack and Stroke Systems. American Heart Association.
- Yanchar N, et al. Chest X-Ray as a Screening Tool for Blunt Thoracic Trauma in Children. J Trauma Acute Care Surg. 2013 Oct.
- Mace SE, Khan N. Needle Cricothyrotomy. Emerg Med Clin North Am. 2008.
- Keller MS, et al. The Utility of Routine Trauma Laboratories in Pediatric Trauma Resuscitations. Am J Surg. 2004.
- Acker SN, Kulongowski AM. Error Traps and Culture of Safety in Pediatric Trauma. Semin Pediatr Surg. 2019 Jun.
- Leidel BA, et al. Is the Intraosseous Access Route Fast and Efficacious Compared to Conventional Central Venous Catheterization in Adult Patients Under Resuscitation in the Emergency Department? A Prospective Observational Pilot Study. Patient Saf Surg. 2009 Oct 8.