Ingestion
Objectives
Upon finishing this module, the student will be able to:
- Describe the fundamental principles of the management of the child with acute overdose.
- Define the differences between the toddler and the adolescent overdose patient.
- Choose the correct gastrointestinal decontamination procedure for the overdose patient.
- Identify when antidotes are indicated.
Contributors
Update Authors: Shan Yin, MD, MPH; Morgan Robinette; and Lilia Reyes, MD.
Original Author: Lilia Reyes, MD.
Update Editor: Navdeep Sekhon, MD.
Original Editor: S. Margaret Paik, MD.
Last Updated: July 2024
Introduction
Poisoning is one of the most common medical emergencies encountered by young children. It accounts for a significant number of ED visits in the adolescent age group. Poisoning may be intentional or unintentional. Unintentional poisonings make up 80-85% or more of all poisoning exposures in children, while intentional poisoning is usually seen in adolescents and young adults and comprises about 10-15% of poisoning cases.
Ingestions in Children Under Five
Among children five years of age and under, most exposures are due to exploratory behavior or willful child abuse. Children between the ages of one to four years have increased finger-mouth activity and/or pica, putting them at greater risk for accidental ingestion. Male gender and a temperament that leans toward hyperactivity are also risk factors. Ingestion is usually of a single agent and in a small amount. Morbidity and mortality are uncommon. Common ingestants in this age group include medications, consumer products, cleaning substances, and foreign bodies. Household cleaning products are the most common exposure in the younger (under five years old) pediatric patient. The most common pharmaceutical ingestions are analgesics, and the most common fatal ingestions are from ethylene glycol, lithium, morphine, tramadol, and disc batteries. A number of poisons (but not a complete list) that are dangerous at small doses include calcium channel blockers, camphor/clonidine, cyclic antidepressants, loperamide, opiates, salicylates, sulfonylureas, and toxic alcohols.
Ingestions by Adolescents
Ingestions in adolescents and young adults are more often self-harm attempts. Ingestion by an adolescent may involve many substances in larger amounts, with morbidity and mortality being more likely. Ingestants are typically medications, with the most common ingestion being acetaminophen and the most fatal ingestion being from cardiac active agents.
Evaluation of the poisoned child begins with the ABC’s of resuscitation and stabilization: assess airway, breathing, and circulation. If the patient is unstable, then the history and physical should be done concurrently with the resuscitation. The most common approach in the poisoned child/adolescent who has a decreased level of consciousness or abnormal vital signs is to address the few reversible causes for the symptoms presented. Initial steps include:
- If there is hypoxia, place the patient on oxygen via a nonrebreather.
- Patients with hypotension should be given crystalloid fluid boluses (20cc/kg) or a vasopressor agent if crystalloid fluid resuscitation fails to correct the hypotension.
- If there is evidence of hypoglycemia from a finger stick blood glucose, give intravenous dextrose (D10W 5cc/kg/dose) as needed.
- Consider giving naloxone 0.1mg/kg/dose IV (max 2mg) in the unresponsive patient with respiratory depression and suspected opiate ingestion, although some patients may require more than 2mg total.
- Early consultation with a regional poison center and/or a medical toxicologist should be initiated, especially for patients with more than minor symptoms.
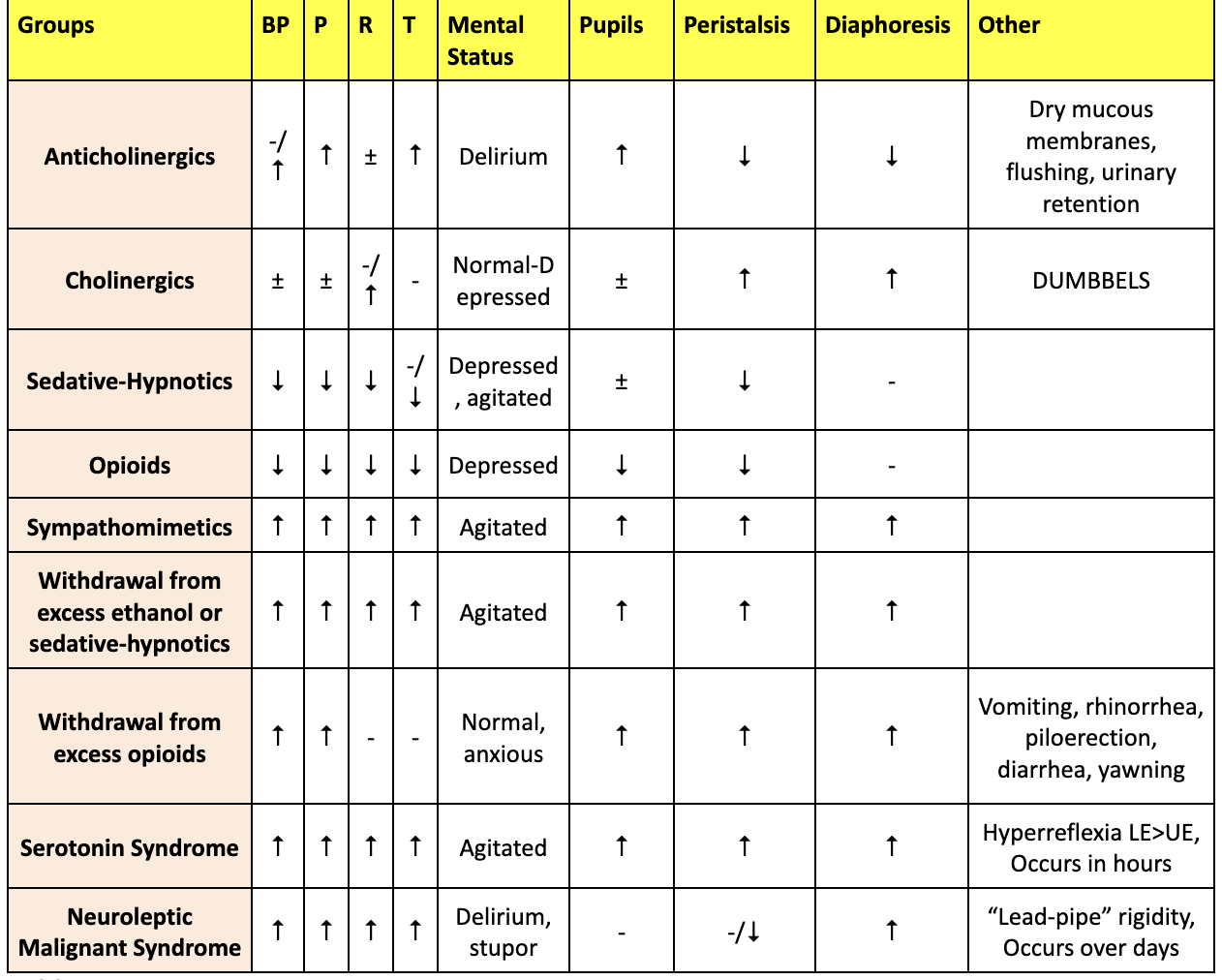
The presentation of ingestion varies greatly depending on the substance ingested. However, there are several common toxic syndromes, or toxidromes, that consist of certain signs and symptoms associated with a particular class of ingestant. The five most common toxidromes are anticholinergic, cholinergic, opioid, sedative-hypnotic, and sympathomimetic. It is helpful to be able to recognize toxidromes rapidly, as early recognition can help determine if a specific agent or type of poison is involved.
It is important to note the classic presentation may not always be present and furthermore, polypharmacy ingestions may affect the presentation. For example, mixing amphetamine and opioids (often called a "speedball") may produce antagonistic signs or symptoms. Additional toxic syndromes include serotonin syndrome, neuroleptic malignant syndrome, and malignant hyperthermia. Lastly, while withdrawal syndromes are not toxidromes, their presentation can appear very similar to toxidromes and should be considered in the differential. It is also important to recognize that some ingestants, such as acetaminophen, may initially present asymptomatically but can cause patients to decompensate later. In cases of suspected ingestion, Poison Control can be a helpful resource for both families and clinicians.
Anticholinergic
The anticholinergic toxidrome classically presents with signs of decreased or inhibited parasympathetic activity, such as: altered mental status, mydriasis, hyperthermia, or dry/flushed skin.
Cholinergic
Cholinergic poisonings cause an over-activation of the parasympathetic nervous system, leading to several symptoms that can be remembered with the acronyms SLUDGE and DUMBBELS.
SLUDGE
- Salivation
- Lacrimation
- Urination
- Defecation and Diaphoresis
- Gastrointestinal Upset
- Bradycardia or Tachycardia (depending on if the ingestant is muscarinic or nicotinic)
DUMBBELS
- Defectation and Diaphoresis
- Urination
- Miosis
- Bronchorhea, Bronchospasm, and Bradycardia
- Emesis
- Lacrimation
- Salivation, Seizures
Sympathomimetic
Sympathomimetic poisonings commonly activate a fight-or-flight response in patients. Symptoms include: agitation, tachycardia, hypertension, hyperthermia, sweating, mydriasis, seizures, and hallucinations.
Opioid and Sedative-Hypnotic
Opioid toxidromes present with decreased mental status, pinpoint pupils (miosis), and respiratory depression. Sedative-hypnotic poisonings present similarly to the opioid toxidrome but without miosis.
History
It is important that you ask what medications are in the home, both prescription and over the counter. If you are able to identify what the substance is, you should ask for the following information/questions:
- What time did the ingestion happen?
- How much of the medication was in the container originally?
- How much medication was left at the time of presentation?
- What symptoms have the patient had since ingestion?
Physical Examination
- Vital Signs.
- Level of Consciousness.
- Pupils: Miosis or mydriasis.
- Skin: Color, presence of diaphoresis, dry skin, or piloerection. The best place to check for anhydrosis is under the armpit or in the groin.
- Oral: Moist/dry mucous membranes.
- Abdomen: Hyper- or hypoactive bowel sounds, bladder size (urinary retention).
- Neurological: Hypo- or hyperreflexia, seizures.
- Odors: Certain ingestions are associated with specific odors (for example cyanide may have a bitter almond odor).
Toxidromes are a set of signs and symptoms seen in specific poisonings. These become clinically applicable in poisonings regardless of an available antidote. Life-saving antidotes are available for opioids, tricyclic antidepressants, and cholinergic ingestions. Common toxidromes are listed below, as well as specific antidotes for common agents.
Common Toxidromes
| Opiate | Sympathomimetic | Anticholinergic | Cholinergic | Sedative-Hypnotic | |
| Examples | Heroin, Morphine, Clonidine | Cocaine, Amphetamines | Antihistamines, Tricyclic antidepressants, Some antipsychotics | Organophosphates, Nerve agents, Mushrooms (muscarin-containing) | Benzos, Barbiturates |
| Mental Status | Decreased | Increased | Increased | Decreased | Decreased |
| Pupils | Miosis | Mydriasis | Mydriasis | Miosis | Miosis |
| HR | Bradycardia | Tachycardia | Tachycardia | Bradycardia | |
| BP | Hypotension | Hypertension | Hypertension | Hypotension | |
| RR | Apnea | Tachypnea | Tachypnea | ||
| Temp | Hypothermia | Hyperthermia | Hyperthermia | Hypothermia | Hypothermia |
| Physical Exam | Sedation, Clammy skin, Cyanosis of lips and nails, Emesis | Tremor, Diaphoresis, Warm skin, Hyperactive bowel sounds, Hyperreflexia | Dry/flushed skin, Urinary retention, Hypoactive bowel sounds | Salivation, Lacrimation, Urination, Defecation, Diaphoresis, Emesis, Bronchorrhea, Muscle fasciculation | Hypoactive bowel sounds, Hyporeflexia |
| Treatment | Naloxone | Benzodiazepine | Physostigmine | Atropine Pralidoxime | Supportive |
Vital Sign and Physical Exam Findings in Common Toxidromes
Common Ingestion Agents and Antidotes
| Agent | Antidote |
| Acetaminophen | N-acetylcysteine |
| Carbon Monoxide / Carboxyhemoglobin | Oxygen, Hyperbaric oxygen |
| Ethylene Glycol / Methanol | Fomepizole, Ethanol |
| Iron | Deferoxamine |
| Lithium | No specific agent - GI decontamination, Hemodialysis |
| Methemoglobin | Methylene blue |
| Salicylates | Urine alkalinization |
| Opioids | Naloxone |
| Sulfonylureas | Ocreotide |
The most common type of toxicology screen used in hospital settings is a series of immunoassays for a select number of common ingestants. Urine is most often the medium used for such screens, as it is easy to obtain in large quantities and analyze. However, urinary toxicology screens are generally not helpful in the initial management of patients, as there may be false positives or negatives. In addition, a positive screen only shows evidence of exposure and cannot be used to confirm intoxication. Additionally, urinary toxicology screens are also not standardized from one institution to another, and some ingestants, like toxic alcohols and organophosphates, are not usually included in the series of immunoassays.
Certain EKG findings, particularly in the QRS and QT intervals, as well as R-waves and dysrhythmias, can be helpful in diagnosis and management of an ingestion. EKGs should be ordered empirically for all self-harm ingestions.
Basic laboratory tests can be useful in identifying toxins that may cause a characteristic abnormality. Patients with anion gap metabolic acidosis or an osmolar gap have a common differential diagnosis that should be evaluated as part of the work up. Importantly, a normal osmol gap does not rule out a toxic alcohol ingestion. MUDPILES is an often-used mnemonic for remembering causes of metabolic acidosis, but it is important to note that it is not an exhaustive list.
- Methanol
- Uremia
- DKA
- Paraldehyde
- Iron, Isoniazid
- Lactic Acid
- Ethylene Glycol
- Salicylate
Agents that cause an osmolar gap include ethanol, lactic acidosis, isopropanol, alcoholic ketoacidosis, methanol, renal failure, ethylene glycol, ethyl ether, acetone, and paraldehyde.
- Osmolar gap = (measured osmols - calculated osmols)
- Calculated osmols = {(2Na) + (Glucose/18) + (BUN/2.8)}
Serum drug concentrations for certain agents have levels that correspond to toxicity and have specific antidotes. Acetaminophen and salicylates should be screened for in most cases of ingestions as they are common ingestions and coingestants. Utility of the serum concentration is dependent on clinical correlation as well as other factors including timing of ingestion, mechanism of action, duration of effect, toxicokinetics, and toxicodynamics. Below is a list of drugs that have measurable toxicity levels and have a specific antidote:
- Acetaminophen
- Carbon Monoxide / Carboxyhemoglobin
- Ethylene Glycol
- Iron
- Lithium
- Methanol
- Methemoglobin
- Phenytoin
- Salicylates
- Valproic Acid
The management of the poisoned patient acutely should focus on supportive care (i.e. A, B, C’s). In specific situations enhancing elimination and/or specific antidotes may be indicated. Preventions of absorption can be accomplished by expelling toxin from above or below or via urinary alkalinization. Despite its widespread use, gastrointestinal decontamination has not been demonstrated to be beneficial in clinical trials.
The purpose of gastric decontamination is to prevent the systemic absorption of a toxin that is in the GI tract. While gastric lavage has largely fallen out of favor, there may be isolated cases in which it is indicated. While the few large, randomized trials with activated charcoal do not show a benefit, they suffer from methodological deficiencies. Smaller studies on single agents as well as volunteer studies do show a benefit and activated charcoal should be considered for ingestions as long as there are no contraindications. There is no single time from initial ingestion for which charcoal cannot be given and timing depends on the substance. For example, the benefit of activated charcoal with salicylate ingestions likely extends far past one hour.
Mechanisms of Decontamination
Syrup of Ipecac
- Mechanism: Plant extract that causes emesis.
- Indications: No longer recommended.
- Contraindication: Acids, alkalis, hydrocarbons, unprotected airway, depressed level of consciousness, seizure, cardio-pulmonary instability.
- Complications: Aspiration, esophageal rupture, protracted vomiting.
Orogastric Lavage
- Mechanism: Use of large bore OG tube - gastric irritation to remove pill fragments.
- Indications: No longer recommended by the American Academy of Clinical Toxicology. Consider its use for a life-threatening ingestion for which there is no specific treatment, consultation with a regional poison center is advised.
- Contraindication: Acids, alkalis, hydrocarbons, unprotected airway.
- Complications: Aspiration, esophageal rupture.
Activated Charcoal
- Mechanism: Absorption by charcoal prevents absorption of drug in the GI tract.
- Indications: Ingestion of potentially toxic amount of a substance within one hour of presentation. Can be given past one hour based on the substance.
- Contraindication: Absence of intact or protected airway, bowel obstruction/perforation. Should not be administered by NG unless intubated. Things not absorbed by charcoal include acids/alkali, hydrocarbon, heavy metals (lithium, iron), cyanide, pesticides, solvents, and alcohols.
- Complications: Aspiration.
- Dose: 1gm/kg PO/NG (child), 50-100gm (adolescent/adult). Recommended dosage can also be 10:1 ratio of activated charcoal to poison ingested.
Multi-Dose Activated Charcoal
- Mechanism: Uses GI tract as a dialysis membrane.
- Indications: Agents with enterohepatic or enteroenteric circulation, such as carbamazepine, digoxin, valproic acid, phenobarbital, salicylates, and theophylline.
- Contraindication: May not be indicated in digoxin ingestion. Salicylate ingestion may require more than one dose but not multiple doses.
Cathartics (Sorbitol)
- Mechanisms: Hyperosmolar agent that increases stool output.
- Indications: Little evidence to support its use and generally not an option for gastric decontamination.
- Contraindication: < six years old.
- Complications: Electrolyte abnormalities.
Whole Bowel Irrigation
- Mechanism: Large volumes of polyethylene glycol are used to flush GI tract without causing fluid/electrolyte abnormalities.
- Indications: Useful for iron, lithium, and sustained release/enteric-coated preparation. Consider its use for drug packers.
- Contraindication: Ileus, GI obstruction/perforation, colitis.
- Dose: 25mL/kg/hr for a child (max 400mL), 1-1.5L/hr for an adolescent/adult.
Ion Trapping (Urinary Alkalinization)
- Mechanism: Alkalinizing the urine may enhance excretion of acids by using H+ ions, which leaves the toxin in its ion form that decreases aborption and promotes excretion. Perhaps more importantly, alkalinization can promote movement of the substance out of the CNS and into the serum.
- Indications: Salicylate or phenobarbital ingestions.
- Complications: Must maintain normokalemia. Hypokalemia will decrease the potassium/acid exchange in the kidneys.
- Dose: 1-2mEq/kg NaHCO3 3-4hrs (goal urine pH 7.0-8.0).
Hemodialysis
- Mechanism: Direct removal of toxin from the blood and corrects metabolic derangements.
- Indications: Use for toxins that are small, have low protein binding, and have a low volume of distribution. Failure of supportive care and antidotes (e.g. ethylene glycol, lithium, methanol, phenobarbital, salicylates, and theophylline).
In summary, this is the general approach to the management of the poisoned pediatric patient.
- Resuscitation.
- Assess airway and intubate if needed.
- Assess breathing and maintain oxygenation/ventilation.
- Give naloxone for respiratory depression due to suspected opiate intoxication.
- Assess circulation and maintain cardiopulmonary monitoring. Fluid resuscitate with crystalloid if in shock.
- Assess disability (i.e. mental status, seizures). Check for hypoglycemia. Remove clothing and place in plastic bag for patients with dermal exposures.
- Assess environment for possible child abuse, suicidal intent, or substance abuse.
- Clinical Evaluation (history/physical exam) to determine likely substance and substance class.
- Consider gastric decontamination, if appropriate.
- Testing.
- Screen for acetaminophen, salicylates, and pregnancy (if female) in all ingestions.
- Obtain CBC, BMP, blood gas, bedside blood glucose, and specific drug levels ad indicated.
- EKG may show signs of toxicity.
- Chest x-ray for respiratory depression (i.e. aspiration pneumonitis, pulmonary edema).
- Abdominal x-ray for suspected ingestion of iron, enteric-coated preparations, or heavy metal.
- Administer specific antidotes as indicated.
- Consider toxin elimination techniques.
- Supportive care.
Pitfalls
- Failing to recognize that the history is usually by far the most important aspect of identifying the toxin.
- Failing to link physical exam findings to a possible toxidrome, which could delay identification of an appropriate therapy.
- Failure to use activated charcoal in the management of the appropriate poisoned patient and relying on "one hour" as dogma.
- Failing to identify concerning EKG findings that would need intervention, as in the case of TCA, calcium, and beta blocker toxicity.
- Forgetting to use anion gap and osmolar gap calculations to identify possible toxins.
- Neglecting to monitor urine pH when using sodium bicarbonate to treat salicylate poisoning.
- Forgetting to order an acetaminophen and salicylate level on ingestions, as they are common ingestions and coingetants. Remember that the Rumack-Matthew Nomogram starts at four hours after ingestion.
- Failure to consult the poison center when appropriate.
The father and child permit the nurse to collect blood from the four-year-old patient. One hour later, the RN reports to you that the child has started vomiting and is asking for some Zofran. The lab calls you five minutes later with a critical lab value, the patient's acetaminophen level is 300 micrograms/mL.
You check the Rumack-Matthew Nomogram and note that this level is above the treatment level. You start the N-acetylcysteine and the father profusely thanks you for advocating for the needed testing.
- Bryant S, Singer J. Management of Toxic Exposure in Children. Emerg Med Clin North Am. 2003.
- Emery D, Singer J. Highly Toxic Ingestions for Toddlers: When a Pill Can Kill. Pediatr Emerg Med Rep. 1998.
- Henretig, FM. Special Considerations in the Poisoned Pediatric Patient. Emerg Clin North Am. 1994.
- Michael JB, Sztajnkrycer MD. Deadly Pediatric Poisons: Nine Common Agents that Kill at Low Doses. Emerg Med Clin North Am. 2004 Nov.
- Osterhoudt KC, Burns-Ewald M, et al. Toxicologic Emergencies. Textbook of Pediatric Emergency Medicine. Lippincott Williams & Wilkins. 2010.
- Alvarez A. Poisonings. M4 Curriculum. Society for Academic Emergency Medicine (SAEM). 2019.
- Weier A, Kleinschmidt K. How are Patients Admitted to the ICU After Common Poisonings Diagnosed and Managed? Evidence-Based Practice of Clinical Care. 2010.
- Bhalla A. Bedside Point of Care Toxicology Screens in the ED: Utility and Pitfalls. Int J Crit Illn Inj Sci. 2014.
