Altered Mental Status
Objectives
Upon finishing this module, the student will be able to:
- Learn to recognize signs of altered mental status in children.
- Develop a differential diagnosis for altered mental status, including unique causes to pediatrics.
- Review initial steps in resuscitation of a pediatric patient with altered mental status.
- Consider basic and specialized testing in the work-up of altered mental status in the pediatric patient.
Contributors
Update Author: Emily Wagner, MD
Original Author: Keith Henry, MD
Update Editor: Aman Pandey, MD
Original Editor: S. Margaret Paik, MD
Last Updated: July 2024
Introduction
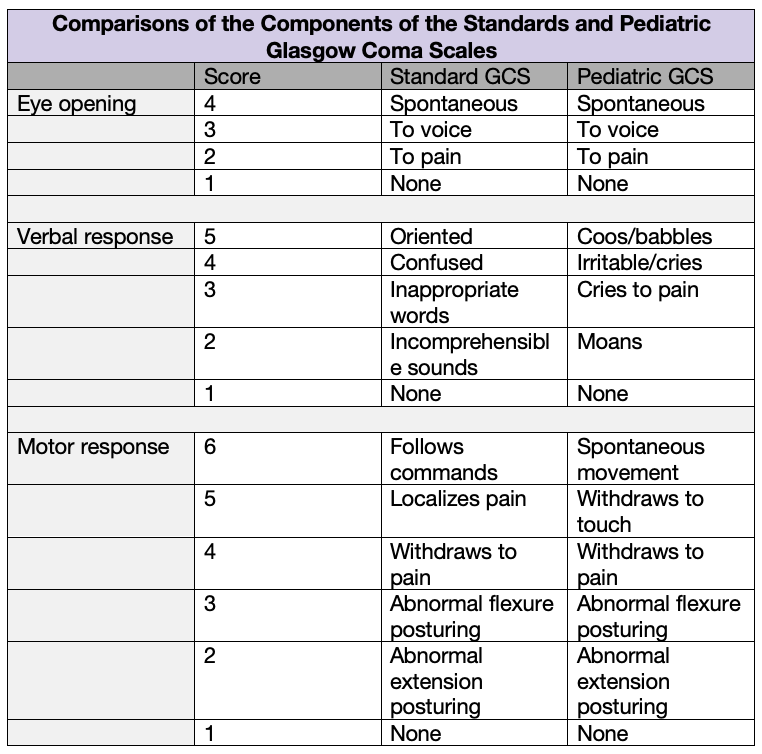
Recognizing altered mental status in a pediatric patient, especially in infants, can be enormously difficult. As with any initial emergency department (ED) encounter, learners should begin by completing the primary survey. Learners should have an awareness of the differences between the adult and pediatric Glasgow Coma Scale (GCS), shown below. While often used in evaluation of traumatic injuries, its components also commonly serve as a standardized assessment tool used during the initial triage and resuscitation process of any patient with mental status changes (Pearl: it is important to note that the lowest GCS score possible is three - even a deceased patient has a GCS of three).
After completion of the primary survey, learners should focus on obtaining a thorough history. This includes asking caregivers about a patient's baseline level of function (e.g. is the patient verbal or nonverbal? Is the patient ambulatory or non-ambulatory?). Learners should have a solid grounding in each of the five domains of normal pediatric developmental milestones to help guide their hypothesis-driven history taking.
If a pediatric patient is determined to be altered, resuscitation and work-up should not be delayed. Initial actions and special considerations:
- Obtain vital signs and place on monitor.
- Assess Airway: Is their airway clear? Any signs of choking or respiratory distress that could indicate a respiratory compromise as a cause of altered mental status due to hypoxia or hypercarbia? Is there emesis or copious secretions?
- Assess Breathing: Is the patient breathing normally on their own? Is there any pattern of abnormal breathing (such as Kussmaul breathing or abnormal respirations as part of Cushing's triad for elevated intracranial pressure)?
- Assess Circulation: How strong are pulses? Capillary refill? Is there mottling present to suggest causes of altered mental status such as shock?
- Disability: Is the patient acting appropriately? Are they responsive to noise or physical stimuli? What is the patient's tone like? Are they moving extremities symmetrically? If they can walk at baseline, what is their gait currently? Do they have a seizure history?
- Special Considerations: Any signs of trauma? In an infant, are there any signs of a bulging or sunken fontanelle?
- IV Access: Establish early intravenous or intraosseous access in the critically ill child.
- Obtain Point of Care Glucose. This is a common cause of altered mental status in children and should be corrected as quickly as possible. Causes of hypoglycemia can vary and should be addressed in the differential diagnosis and testing.
The pediatric patient with altered mental status can vary greatly. Age and verbal status of the patient contribute greatly to their baseline mental status as well as any change in mentation. It is extremely important to ask caregivers about the child’s normal baseline mental status and behavior. For example, a patient with cerebral palsy may not walk or talk at baseline but they still may be less interactive than usual per the report of the caregiver. It’s important for the clinician to recognize the caregiver’s familiarity with the patient's baseline when obtaining the history. Changes from the patient’s baseline may seem subtle or even non-existent to an expert clinician but may be obvious to the experienced caregiver. It may be easier to consider signs of altered mental status by age:
Infant
- May be sleepier than usual. Is the infant waking to feed? When they are awake, are they interactive as usual?
- Breathing may be abnormal in the obtunded patient. Is their breathing irregular? Is it faster or slower than usual?
- Look for abnormal tone. Tone is very important. Many babies with altered mental status present with hypotonia. A floppy baby is a sick baby.
- Assess the anterior fontanelle. Both sunken and bulging fontanelles are concerning.
- Non-accidental trauma must be considered. Any skin finding that could be consistent with bruising or burns should be noted. Oral frenulum tears, while rare, are also highly concerning.
Toddler
- May be sleepier than usual or napping outside of usual times.
- In the walking toddler, gait or balance may be abnormal.
- Speech may be unusual (with respect to patient's age and reported baseline).
- Look for abnormal tone.
School Age Child and Older
- May be sleepier than usual.
- Can often provide slightly more history on their own regarding other symptoms such as headache, abdominal pain, or history of trauma.
- Tone and gait may be abnormal.
- Confusion or abnormal speech may be present.
The differential diagnosis for altered mental status for children is vast. The well-known mnemonic AEIOU TIPS can be applied to the pediatric population, with a few additional diagnoses that are special to children.
- A: Alcohol, ammonia
- E: Epilepsy, electrolyte disturbances, endocrine disorders
- I: Infection, intussusception, ischemia
- O: Overdose, oxygen deficiency
- U: Uremia
- T: Trauma (both accidental and non-accidental), temperature abnormality, tumor, thyroid dysfunction
- I: Increased intracranial pressure, insulin-related problems
- P: Poisoning, psychiatric conditions, perfusion (e.g. hypertension or hypotension)
- S: Shock, stroke, space-occupying CNS lesion, shunt problem
Basic
- Point-of-care glucose test immediately.
- Labs including a basic metabolic panel to check electrolytes, complete blood count to assess for infection, bleeding, and platelet count.
- Head imaging, if severely altered or obtunded. Initially obtain a CT Head without IV contrast as it is a rapid diagnostic tool and does not require sedation. Consider rapid Brain MRI without contrast if this is available (institution-dependent). May require a sedated Brain/Spine MRI for further work-up after initial stabilization.
Specialized
- If febrile: Blood cultures. Lumbar puncture with CSF profile with cell count and differential, protein, glucose, Gram stain, meningo-encephalitis panel. Consider HSV PCR in both CSF and blood in infants. Consider specialized blood tests for infections such as mosquito- or tick-borne illnesses based on history.
- If concern for toxidrome or ingestion: Acetaminophen/aspirin levels, EKG, hepatic panel, INR (consider urine drug screen for marijuana and some opiates), lactate.
- If concern for metabolism/endocrine disorder: Hepatic panel, ammonia, lactate, urine organic acids, TSH with reflex T4, beta-hydroxybutyrate, urine ketones.
- If abdominal pain: Urinalysis, abdominal ultrasound for intussusception, abdominal x-ray for volvulus or pneumatosis, abdominal CT for appendicitis or bowel ischemia.
- If concern for shunt malfunction: Consultation with neurosurgery for possible shunt interrogation, order a shunt series x-ray and head imaging according to local protocol (usually CT Head or rapid Brain MRI).
- If intracranial bleeding and/or bruising: Obtain coagulation tests, discuss further work-up with child abuse pediatrician.
Treatment will largely depend on the cause of altered mental status.
- Hypoglycemia can be treated with IV dextrose but the cause should be investigated.
- Intracranial findings, whether oncologic or traumatic, generally require neurosurgical consultation. In the decompensating child, consider early hypertonic saline or mannitol administration.
- If diabetic ketoacidosis is suspected, altered mental status can indicate cerebral edema. Consult a pediatric critical care physician to determine fluid resuscitation goals and insulin-dosing if possible.
- If infection is suspected, begin empiric treatment with broad-spectrum antibiotics (and acyclovir if indicated) as soon as possible. This is a very common cause of altered mental status in infants and toddlers.
- Treatments for toxidromes will depend on the agent ingested. Call the local Poison Control Center or consult with toxicology early if intentional or accidental overdose is suspected.
- Pediatric metabolic conditions often require specialized fluid resuscitation and other specialized treatment interventions such as carnitine or ammonia scavengers. Consult a pediatric metabolic specialist early in the resuscitation of these patients.
- Abdominal pain as the cause of altered mental status usually requires surgical intervention and empiric antibiotics.
Pearls
- Altered mental status in infants and children can vary by age and by the patient's baseline. The caregiver's history will often provide the most valuable tools in making a diagnosis.
- The differential diagnosis for altered mental status in children is huge, and the mnemonic AEIOU TIPS may be helpful to review both common and uncommon causes.
- Address the ABCs in a critically ill child but don't forget to check the glucose.
- Treatment of the infant or child with altered mental status is dependent on the cause, but infection is common. Administer early empiric antibiotics if the patient is febrile or if concern for infection is high.
Pitfalls
- An accurate assessment cannot be made without knowing a patient's baseline. Having no diagnosis is often safer than a misdiagnosis that's based on poor information.
- Failure to walk a patient or wake a patient will miss the true degree of obtundation or change from baseline.
- Failure to consult a pediatric specialist early in the course of an endocrine or metabolic disorder may cause the patient harm during resuscitation efforts.
- Borgialli DA, et al. Performance of the Pediatric Glasgow Coma Scale Score in the Evaluation of Children with Blunt Head Trauma. Academic Emergency Medicine. 2016.
- Dunnick J, Herman B, Rose JA. Pediatric Emergencies Presenting to Urgent Care Centers. Urgent Care Medicine. 2017.
- Levene RJ, Pollak-Christian E, Wolfram S. A 21st Century Problem: Cannabis Toxicity in a 13-Month-Old Child. The Journal of Emergency Medicine. 2019.
