Abdominal Trauma
Author Credentials
Author: Nur-Ain Nadir. MD. Kaiser Permanente Central Valley, Kaiser Permanente School of Medicine.
Editor: Gregory J. Tudor, MD, University of IL College of Medicine - Peoria, IL
Last Revised: November 2019
Case Study
You are in the middle of your shift and overhear an EMS call regarding a trauma patient coming in with lights and sirens: “Onboard we have a 23 year-old male, stabbing victim with a single stab wound to the abdomen, multiple abrasions, contusions and lacerations to the extremities. He is awake and protecting his airway, but his abdomen is distended and his blood pressure is 90 palpated, pulse of 118, and respiratory rate of 24. We are working on getting an IV now. ETA is 4 min.” You realize that you are next up for a patient assignment and run through your mental checklist for abdominal trauma: What organs are most likely to be injured given this mechanism? Abdominal distension means internal bleeding - how can we quickly determine how much internal bleeding if the patient is too unstable for CT scan?
Objectives
Upon completion of this module, the student will be able to:
- Understand how to diagnose, resuscitate, stabilize and manage abdominal trauma patients.
- Identify common pathophysiologic conditions in abdominal trauma.
- Describe the components of a primary survey in a patient with abdominal trauma.
- Generate a differential diagnosis of potential traumatic injuries based on history, mechanism, and physical exam.
- List commonly utilized imaging modalities in abdominal trauma.
- Discuss the eventual disposition of abdominal trauma patients based on their diagnosis.
- Appreciate the necessity for emergent surgical intervention in certain abdominal trauma conditions
Introduction
Abdominal trauma is seen quite often in the Emergency Department and can result from blunt or penetrating mechanisms. Blunt abdominal trauma (BAT) is frequently encountered in the form of motor vehicle crashes (MVCs) (75%), followed by falls and direct abdominal impact.
Three kinds of forces are seen with BAT:
- shearing forces that occur due to rapid deceleration causing tearing at fixed points of attachments;
- crushing forces that cause intra-abdominal contents to be crushed between anterior abdominal wall and posterior structures, ribs and vertebrae;
- external compression which causes the sudden and rapid rise in intra-abdominal pressure leading to rupture of hollow viscus organs.
Penetrating abdominal trauma (PAT) is on the rise with increasing gang violence. There are two main kinds of PAT: Stab Wounds (SW) and Gun Shot Wounds (GSW). SWs are more common than GSWs, however they have a lower mortality rate compared with GSWs. The higher energy transfer and missile trajectory with multiple bullet fragments from GSWs leads to increased morbidity and mortality compared to stab wounds.
Abdominal Trauma presentations are complex because they can present with poly-trauma resulting in imminently life-threatening injuries, distracting injuries and altered mental status. This can make the diagnosis of abdominal traumatic injuries even more challenging.
Initial Actions and Primary Survey
Abdominal trauma can present in multiple ways. Patients brought by Emergency Medical Transport are typically immobilized with spine-board and cervical-collar precautions. Patients may also present via private vehicle, in which case the prudent plan of action is to rapidly assess the ABCs while applying spinal immobilization and proceeding in accordance with ATLS guidelines. Of note, occult cervical spine injury is unlikely in patients with penetrating trauma. Unless there is a deficit or concerning mechanism (blunt trauma combined with penetrating trauma), a cervical collar is rarely necessary and may hinder treatment in penetrating trauma victims.
All trauma patients must be managed in accordance with the Advanced Trauma Life Support (ATLS) algorithm:
- A: Airway Maintenance with CERVICAL SPINE protection (Is the patient speaking in full sentences?)
- B: Breathing and Ventilation (Is the breathing labored? Bilateral symmetric breath sounds and chest rise?)
- C: Circulation with hemorrhage control/shock assessment (Pulses present and symmetric? Skin appearance: cold & clammy or warm & well perfused?)
- D: Disability (GCS score? Moving all extremities?)
- E: Exposure/Environmental Control (Completely expose the patient)
If the patient’s primary survey is intact, the adjuncts to the primary survey and resuscitation begin. The adjuncts to the primary survey include any of the following as necessary: eFAST exam, EKG, ABG, chest X-ray, pelvis x-ray, and/or urinary catheter. Bedside sonography should be used to perform an eFAST exam (Figure 1 ). Figure. 2 demonstrates a negative RUQ eFAST exam. In the setting of hypotension, free fluid on the eFAST exam suggests hemoperitoneum, which suggests the need for emergent surgical intervention (see Figure 3). There a numerous tutorial videos demonstrating eFAST exams. One can be found here that has a large number of video clips of both positive and negative exams.
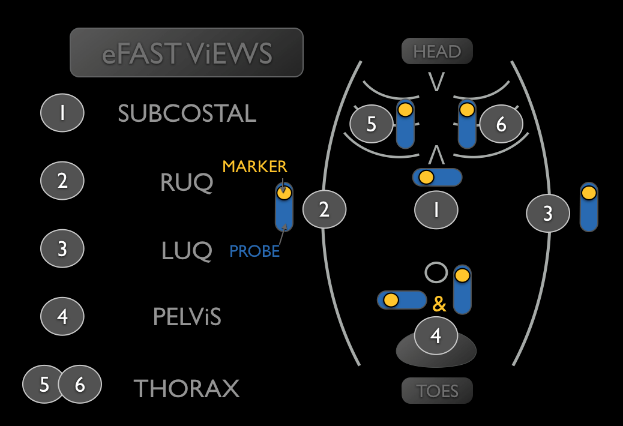
Fig 1. US probe position of an eFAST exam. Note the order that the exam should be performed in. Original image from https://sofsono.org/core-concepts/efast/.
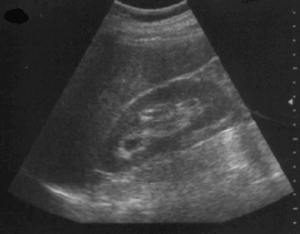
Figure 2: Normal FAST exam window showing the liver and the spleen in a view of the right upper quadrant. Images courtesy of Dr. David Bahner, MD, Associate Professor of Emergency Medicine, The Ohio State University Department of Emergency Medicine. CC BY4.0
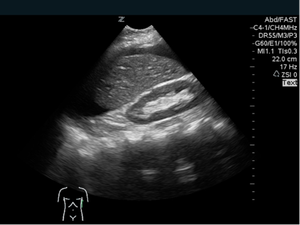

Figure 3: Positive FAST image of LUQ courtesy of David Bahner MD, RDMS Associate Professor of Emergency Medicine, The Ohio State University Department of Emergency Medicine. CC BY4.
Details of the abdominal trauma mechanism are helpful. For MVCs speed of collision, position of colliding car to each other, position of patient in the car, seatbelt use, and extent of damage (intrusion, windshield damage, difficulty of extrication, air-bag deployment) are important elements to elicit. With respect to falls, height of fall is very important. In gunshot wounds, the type of gun, distance from the shooter, and number of shots heard are all relevant. For stab wounds, it is prudent to obtain information on the type of weapon used.
The Secondary Survey
Following the primary survey, the secondary survey must be performed. The secondary survey is the complete history and physical examination. This is completed after all aspects of the primary survey have been addressed and vital functions are returning to normal.
Start by taking an “AMPLE” history (Allergies, Medications, Past Medical History, Last Oral Intake and Events Preceding the Incident). The AMPLE history can be obtained at the same time as the physical exam portion of the secondary survey if the patient is alert and cooperative.
The abdomen should be examined by inspection, auscultation, palpation, and percussion. The abdominal exam should detail exit and entry wounds, number of wounds, any evisceration, ecchymosis and deformity, in addition to tenderness. The perineum, rectum and genitalia should all be examined at this point. A rectal exam can alert the provider to a high riding prostate, lack of rectal tone, or heme-positive stools. The stability of the pelvis should also be assessed during the physical exam.
When assessing a trauma victim, it is important to be aware of factors that make a physical exam unreliable. These factors include altered mental status, intoxication and distracting injuries. The most important way to make your physical exam reliable is to perform it serially, noting important changes as the patient is reexamined.
Presentation
Abdominal trauma patients can present in a wide variety of ways ranging from frank shock to hemodynamic instability to completely stable vitals to poly-trauma. An altered mental status makes the diagnosis of abdominal traumatic injury very challenging. Patients can also present in traumatic arrest due to massive abdominal trauma.
Penetrating injuries are easier to detect. Hemodynamically stable patients often complain of abdominal tenderness, and their exams can reveal peritoneal signs. Of the penetrating injuries, GSWs may be deceptive as missile trajectory and entrance/exit wounds may be difficult to predict accurately.
Blunt abdominal traumatic injuries are notoriously more difficult to detect, and patients may present without specific abdominal tenderness or are distracted due to other injuries. Nausea and vomiting may also occur for a variety of reasons that are not associated with intra-abdominal injury.
Injuries Seen in Abdominal Trauma – Differential Diagnosis
Solid and hollow organ injuries may occur in abdominal trauma patients. With blunt trauma, splenic lacerations are the most common injury followed by liver lacerations. Bladder rupture can also be encountered. Intestinal injuries, although less common, may also be present. Blunt abdominal trauma may lead to diaphragmatic rupture, most commonly on the patient’s left side.
Patients with diaphragmatic injuries may present with vague complaints sometimes weeks after the initial accident. A high index of suspicion should be maintained if you are considering a diaphragmatic injury. Pelvic fracture is another common injury seen in blunt abdominal trauma. Depending on the kind of pelvic fracture, pelvic blood vessels can shear leading to retroperitoneal bleeding and significant blood loss.
With GSWs, small intestine and colonic injuries are most common whereas with SWs, liver injuries are predominant. Penetrating injuries however can result in trauma to any organ system within the abdomen and occasionally the chest depending on the trajectory of the bullet/knife. Penetrating thoraco-abdominal injuries can occasionally result in traumatic arrest (see Table 1).
Table 1. Most Commonly Injured Organs in Penetrating Abdominal Trauma
(From most common at top to less common towards the bottom)
Diagnostic Testing
The bedside sonogram (US) has become standard of care when evaluating patients with BAT. Free fluid in Morrison’s pouch is concerning for hemoperitoneum, which may require emergent surgical intervention (See Figure 3). An initially negative eFAST exam, should be repeated if the clinical picture changes during evaluation. Although bedside sonography is also used for evaluation of PAT, its utility is limited especially for the retroperitoneal organs and cannot reliably evaluate for hollow viscous injury.
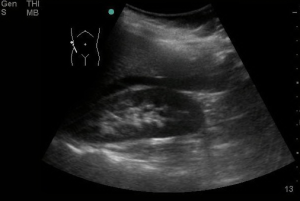

Figure 4: Positive FAST image of RUQ as noted by the arrow. Notice the hypoechoic area between the liver and kidney. Courtesy of David Bahner MD, RDMS CC BY 4.0
For stable patients, the cornerstone of diagnosis is the CT scan with IV contrast. CT scan of the abdomen has excellent sensitivity and specificity in diagnosing both solid and hollow viscus injury. Retroperitoneal organs and the vasculature can also be easily visualized with CT Scans.
The pros of CT scan include the ability to detect intraperitoneal fluid and free air in the abdomen, as well as assessing the solid organs, hollow viscus organs, the retroperitoneum, the vasculature, and the diaphragm. The cons include variable initial interpretation, necessity of patient relocation to CT suite, exposure to ionizing radiation and CT availability.
With respect to blood work, apart from basic labs, type and screen (or when appropriate type and cross) should be sent. Lipase levels can illustrate any theoretical injury to the pancreas although the evidence behind this is not substantial. Urinalysis should be sent to check for signs of hematuria, as this can indicate injury to the genitourinary system. A urine pregnancy test should be obtained in all women of childbearing age.
Treatment
In patients with known abdominal trauma, the patient should receive tetanus vaccination if not up to date. Blood should be transfused as needed, keeping in mind principles of permissive hypotension. Permissive hypotension means avoiding aggressive crystalloid resuscitation of trauma patients, in favor of blood product resuscitation to a specific defined Mean Arterial Pressure (MAP) of 65. Aggressive crystalloid administration to normalize blood pressure may lead to coagulopathy, acidosis and hypothermia which potentiate each other and lead to significant morbidity and mortality. Patients with hollow viscous injury will benefit from antibiotic therapy.
Although simple grade I and II spleen and liver lacerations can often be managed conservatively with observation and blood transfusions, complicated lacerations and grade IV and above injuries often require surgical intervention or embolization by interventional radiology. Intestinal and colonic injuries typically require surgical intervention (exploratory laparotomies). Pelvic fractures with concurrent pelvic vessel injury warrant interventional radiology consultation for emergent arterial embolization. Traumatic aortic injuries warrant judicious blood pressure control and emergent surgical intervention.
Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA)
REBOA is a can be used to help control bleeding and sequester remaining fluid volume in cases of exsanguinating hemorrhage that is below the diaphragm. The REBOA device is inserted using the Seldinger technique under ultrasound guidance into the femoral artery. The catheter is then inserted over a guidewire into the descending aorta as high as zone 1, at the distal thoracic aorta. Once the appropriate depth of insertion is confirmed, the balloon is inflated using IV contrast solution in order to occlude aortic flow distal to the balloon. It is physiologically the same as cross clamping the aorta in a thoracotomy, but does not require opening the chest cavity. Clinical investigations of REBOA suggest potential survival benefit, particularly in patients who are hypotensive but not yet in arrest. REBOA can be used to control hemorrhage in abdominal trauma, as long as there are no thoracic injuries such as aortic dissection or cardiac tamponade (i.e.: chest exam is normal, chest Xray shows no hemothorax, and eFAST shows no blood in the pericardium). Complications include REBOA balloon rupture with loss of vascular control, further or new vascular injury, and end organ ischemia, which in the lower extremities may lead to amputation.
Traumatic arrest due to penetrating thoracoabdominal injuries can be managed with an ED thoracotomy followed by emergent operative intervention. Massive transfusion protocols should be activated. There is no place for ED thoracotomy for blunt thoracoabdominal injuries.
This video is from the manufacturer of one of the catheters as a demonstration of what a REBOA catheter looks like and the procedure.
Disposition
Anyone with identifiable traumatic abdominal injuries on US, and/or CT scan should be admitted to the hospital or transferred to a trauma center for further inpatient monitoring and care. Patients with no identifiable injuries on diagnostic evaluation and continued abdominal pain should be admitted for observation and serial abdominal exams. Patients without identifiable injuries who have a benign physical exam may be discharged home with explicit instructions regarding signs and symptoms that should prompt their return or re-evaluation. There are several occult injuries from BAT including pancreatic, duodenal and bowel injuries that may present in a delayed manner.
Pearls and Pitfalls
- Abdominal trauma patients can present with deceptively unimpressive physical exams yet have significant injuries
- Bedside sonography is increasingly useful for diagnosis of hemoperitoneum in BAT. The presence of free fluid in Morrison’s pouch is pathognomonic for hemoperitoneum.
- An initial negative eFAST may become positive and should be repeated if the clinical picture changes
- GSW penetrating trauma has a much higher morbidity and mortality compared with SW trauma
- Although blunt thoracoabdominal trauma patients are no longer candidates for ED thoracotomies, select penetrating thoracoabdominal trauma patients are candidates for ED thoracotomies
Case Study Resolution
You hear the sirens getting louder as the ambulance carrying your trauma patient pulls into the ED parking lot and recall that a stab wound is most likely to injure: 1. Liver, 2. Small Bowel, 3. Diaphragm or 4. Colon. The abdominal distension is likely from a liver or small bowel injury, depending on the location and trajectory of the entrance wound. You know that eFAST is a quick way to assess for internal bleeding in an unstable patient, even though it’s most helpful in blunt trauma cases; you grab the ultrasound cart on your way to the resuscitation bay. You also know that your trauma surgical team just took a GSW to the OR in the last hour. They might not be available to take this patient to the OR immediately, so you are glad that you just had an in-service training on REBOA. It might just come in handy on this case. The Ambulance crew rolls by and you can see your patient is pale and diaphoretic, but screaming loudly about his abdominal pain, so at least his airway is well protected. You put on a pair of exam gloves and follow them in the room, ready to start your primary survey.
References
- ATLS: Advanced Trauma Life Support for Doctors (Student Course Manual). Ninth ed. American College of Surgeons; 2013.
- Brenner M, Inaba K, Aiolfi A, et al. Resuscitative Endovascular Balloon Occlusion of the Aorta and Resuscitative Thoracotomy in Select Patients with Hemorrhagic Shock: Early Results from the American Association for the Surgery of Trauma’s Aortic Occlusion in Resuscitation for Trauma and Acute Care Surgery Registry. J Am Coll Surg 2018; 226:730
- Holcomb JB, Jenkins D, Rhee P, et al. Damage control resuscitation: directly addressing the early coagulopathy of trauma. Journal of Trauma. 2007;62(2):307-310.
- Isenhour, J.L. & J. Marx. (2007). Advances in abdominal trauma. Emergency Medicine Clinics of North America 25, 713.
- Kman N, Knepel S, Hays HL. “The approach to penetrating abdominal trauma”. Trauma Reports 2012;13 (4): 1-12.
- Knepel S, Kman N, O’Rourke K, Hays HL. 2010. Blunt Abdominal Trauma. Emergency Medicine. Emerg Med 2010;42(8):6-13. (August) http://www.emedmag.com.
- Semenovskaya, Z. & Doty. Chest Trauma. Yakobi, R. et al. (ed). In New York Handbook of Emergency Medicine. (2011).
