Thyroid Storm
Author: Robert W. Wolford, M.D., M.M.M, University of Illinois College of Medicine at Peoria,
Editor: Doug Franzen, MD, M.Ed
Last Update: 2019
Case Study
A 60-year-old female is brought to the Emergency Department by her family because of confusion, fever, and shortness of breath. Her family notes a productive cough and fever that began two days ago. The family states she has been taking aspirin for her fever without improvement. Over the last 24 hours, the patient has become increasingly confused with worsening shortness of breath and has had several episodes of watery, non-bloody diarrhea. Past medical history is only significant for hypertension for which she takes hydrochlorothiazide. Reviewing her medical records finds that she had a routine appointment with her family physician two weeks earlier. At that time, her examination was normal with the exception of a resting sinus tachycardia of 110 bpm. A thyroid stimulating hormone (TSH) level was obtained at that visit and was undetectable. She is scheduled for a follow-up visit with her doctor tomorrow. The patient is only oriented to herself and is unable to provide any additional history or review of symptoms. Vital signs are: Temp 39.4°C, HR 135 bpm, RR 24 bpm, BP 140\45 mmHg, and pulse oximetry on room air of 89%. The cardiac monitor shows atrial fibrillation with rapid ventricular response at 135 bpm. On physical examination she is tachycardic, tachypneic, has diminished breath sounds at the right lung base and diffuse, bilateral crackles, and 2+ pitting edema below the knees. A portable chest radiograph shows a large right lower lobe infiltrate with diffuse interstitial edema.
Objectives
Upon finishing this module, the student will be able to:
- Describe the potential presenting symptoms and signs of thyroid storm.
- List common causes of thyroid storm.
- Discuss the diagnostic approach to thyroid storm.
- Describe the treatment of thyroid storm.
Introduction
Thyroid storm is an uncommon but potentially fatal endocrine emergency at the severe end of the spectrum of thyrotoxicosis. Thyrotoxicosis is thought to affect approximately 1.2% of the United States population and, of those, only 1 to 2% develop thyroid storm. Thyroid storm is more common in women and in the 3rd and 4th decades of life. Thyroid storm typically presents with the signs and symptoms of a hypermetabolic state; however co-existing illnesses, patient age, and the severity of the patient may result in deviations from the classic presentation and potentiate delays in diagnosis. To reduce the morbidity and mortality of thyroid storm, the clinician must consider the diagnosis and implement treatment in a timely fashion. Even with recognition and treatment, mortality is high, ranging from 10% to 75%, although more recent studies found a mortality of 3.6%.
Physiology
A brief review of normal thyroid function follows. Iodide enters the thyroid cells through the sodium iodide symporter and specific thyroglobulin tyrosines are iodinated by thyroid peroxidase, creating mono and di-iodotyrosines. The iodotyrosines combine to form T3 and T4. In response to TSH, T4 and T3 are cleaved from the thyroglobulin and released into the circulation. T4 is the pro-hormone and T3 the active form of the hormone. Eighty percent of the circulating T3 is formed by the conversion of T4 to T3 in the peripheral tissues and the remaining 20% directly released from the thyroid gland. Approximately 99.97 % of T4 and 99.7% of T3 are bound to serum proteins (primarily thyroxine binding globulin) and it is only the free hormones that are metabolically active. Any factor which changes the amount of protein bound hormone (ex. salicylates, diphenylhydantoin, and heparin) may have an impact. Thyroid function is tightly controlled by a negative feedback loop. (Figure 1)
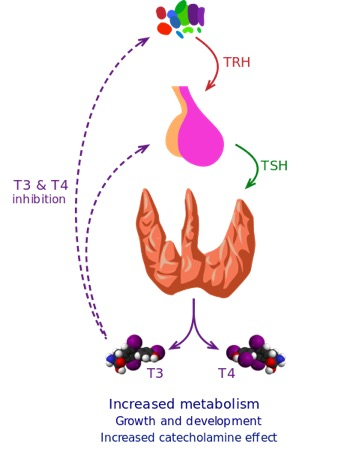
Hypothalamic-Pituitary-Thyroid Axis Wikimedia Commons – Creative Commons Attribution-Share Alike 3.0 Unported no changes made
Initial Actions and Primary Survey
Thyroid storm is exceedingly uncommon in the ED but it should be considered in any patient presenting with a hypermetabolic state, and especially those with a history of thyroid disease. Determining where the symptoms of subacute or chronic thyrotoxicosis end and thyroid storm begins is difficult. The focus of the primary survey and the subsequent detailed history and physical examination is to identify those patients at risk for thyroid storm.
Prior to entering the room, review the vital signs. Fever and tachycardia are common findings in thyroid storm. Tachypnea may be seen, particularly in the setting of complicating heart failure. Hypertension and a widened pulse pressure may also be present. The patient may also be agitated and/or anxious.
ABCs:
Airway: The airway is typically not compromised by thyroid storm. However, these patients are often critically ill and the complications or inciting etiology of the patient’s thyroid storm may require active airway intervention.
Breathing: Tachypnea may occur for numerous reasons: increased basal metabolic rate; underlying heart failure as a complication of long standing thyrotoxicosis (high output heart failure, dilated cardiomyopathy, or cor pulmonale); or other diseases that precipitated thyroid storm (pneumonia).
Circulation: Tachycardia is common, either sinus tachycardia (most common rhythm) or atrial fibrillation (most common dysrhythmia). Supraventricular and ventricular dysrhythmias, including ventricular fibrillation, may occur. A widened pulse pressure and hypertension are frequently seen. However, hypotension and shock may be seen as a complication of the thyroid storm or as a result of the inciting event (e.g. septic shock).
While performing a primary survey, as with any seriously ill patient, the following should be obtained:
- Reliable vascular access, cardiac, SpO2, and BP monitoring. Supplemental oxygen if needed.
- Bedside point–of-care glucose.
- Electrocardiogram.
Presentation
Although the most common presentation is thyrotoxicosis, thyroid storm may be the initial manifestation of the patient’s thyroid disease. Patients classically present with evidence of multisystem decompensation, fever, tachycardia out of proportion to the temperature, and central nervous system dysfunction. Thyroid storm is part of the spectrum of thyrotoxicosis and can be difficult to distinguish from severe thyrotoxicosis. A scoring system has been proposed to identify the likelihood of thyroid storm. Thyroid storm should be near the top of the differential diagnoses for any patient with a history of thyrotoxicosis presenting with CNS dysfunction. Key items to look for on history and physical examination that suggest the presence of thyrotoxicosis and thyroid storm are:
History:
- Is there a history of thyroid disease? If the patient was taking medication for thyroid disease, has the dosage changed recently (including missed doses)?
- Did the patient have subacute or chronic symptoms of thyrotoxicosis that have acutely worsened?
- Are symptoms of thyrotoxicosis found on review of systems? (Table 1)
- Are there new symptoms of depression, or apathy? Often seen in elderly – apathetic hyperthyroidism.
- Has the patient recently started any new medications, had radioiodine, or been given iodinated contrast? (Table 2)
- Any recent physiologic stressors? Infection is the most common trigger of thyroid storm, but also consider surgery, trauma, cardiac events, etc.
A list of common physical exam findings is shown in Table 1.
Other findings include:
- Altered mental status (Spectrum from anxiety and agitation to coma).
- Fine tremor, especially on extension of arms
- Hyperreflexia
- Seizures
- Stare and lid lag are common
- Proptosis, periorbital edema, and chemosis are suggestive of Graves disease
- Enlarged or tender thyroid; thyroid bruit
A thorough exam should target findings suggestive of precipitating causes for decompensation of thyroid disease into thyroid storm (sepsis, stroke, myocardial infarction, etc), as well as complications of thyroid storm such as stroke or congestive heart failure. Common triggers of thyroid storm are listed in Table 3.
Table 1. Symptoms & Signs of Thyrotoxicosis
Table 2. Medication associated thyrotoxicosis. (3)
Table 3. Thyroid storm triggers
To assist in the diagnosis of thyroid storm there are useful clinical calculators. One of these is the Burch-Wartofsky scale. Using the linked calculator can help to predict the likelihood that biochemical thyrotoxicosis is thyroid storm.
Diagnostic Testing
Given the low incidence of thyroid storm, it is critical to maintain a broad differential and evaluate for other possible conditions that would explain the patient’s presentation.
Although thyroid storm is primarily a clinical diagnosis, if thyroid storm is suspected thyroid specific laboratory studies should be obtained and usually include:
- Thyroid stimulating hormone (TSH) level.
- Free thyroxine (T4) level.
- Free triiodothyroxine (T3) level.
Most patients will demonstrate elevated free T4 and T3 levels and a low or undetectable TSH level. The TSH level may be normal in pituitary dependent thyrotoxicosis (pituitary not subject to negative feedback – very rare!). The free T4 may be normal with an elevated free T3 in cases of T3 thyrotoxicosis. The turnaround time for these labs can be hours to days; if thyroid storm is suspected treatment should be started without waiting for confirmatory tests.
Additional tests should be obtained to evaluate for possible precipitating causes (such as a chest radiograph and urinalysis to evaluate for infection) or concurrent conditions (such as electrolytes to evaluate other possible causes of a dysrhythmia, or a BNP to evaluate for heart failure).
Treatment
Patients with thyroid storm are usually critically ill and stabilization should be initiated immediately. These patients are frequently severely volume depleted and require aggressive fluid resuscitation, unless cardiac failure is suspected. Severe hyperthermia should be addressed with cooling and acetaminophen. Salicylates should be avoided as they will displace T4 and T3 from thyroxine binding globulin. Electrolyte abnormalities should be corrected, and dysrhythmias recognized and treated. The inciting etiologies and complications of thyroid storm must be identified and appropriately managed.
Specific treatment for thyroid storm utilizes 3 sequential steps: 1. Block the peripheral effect of the thyroid hormones, 2. Stop the production of hormone in the thyroid, and 3. Stop the release of T3 and T4 from the thyroid. Commonly used medications are listed in Table 5.
Table 5. Medications used in the treatment of thyroid storm. (Adult doses)
Table 5 by Doug Frazen
Peripheral symptom control (ex. tachycardia, chest pain, dyspnea, etc.) is done primarily through β blockade. Traditionally this has been achieved with either oral or intravenous propranolol. However, the serum half-life of propranolol is relatively long (3 to 6 hours) and may worsen symptoms of cardiac failure. Esmolol, with a markedly shorter half-life, may be a better choice in the setting where the patient’s cardiac status is unclear or if the patient has underlying reactive airway disease.
Inhibition of thyroid hormone synthesis is undertaken before inhibition of hormone release. Thioureas, either PTU or methimazole, are used to block additional hormone synthesis. PTU is preferred as it has the additional benefit of blocking peripheral conversion of T4 to T3. PTU is approved for use in pregnancy. However, it does have significant risks, including liver injury and failure and has received a black box warning from the US Food and Drug Administration.
Inhibition of hormone release is achieved with iodine therapy. Iodine therapy should not be started any sooner than one hour after the initiation of a thiourea. In the absence of a thiourea, iodine may actually stimulate release of preformed thyroid hormone. Iodine, in the presence of a thiourea, blocks the release of preformed hormone, decreases iodide transport into thyroid follicular cells, and prevents subsequent oxidation. This inhibition is short lived and ineffective after 48 hours of therapy. Lithium carbonate may be considered in those patients who cannot receive iodine.
Glucocorticoids are also frequently given in thyroid storm as they may decrease the conversion of T4 to T3, although the significance of this effect is unknown. An unknown percentage of patients in thyroid storm also have adrenal insufficiency. Dexamethasone is typically preferred due to its lack of interference on an ACTH stimulation test. A random cortisol level should ideally be obtained prior to administration of a steroid.
All patients in thyroid storm should be admitted to an intensive care unit after stabilization and initiation of thyroid specific interventions. Even with aggressive care, a significant percentage of patients will die.
Case Study
The patient is diagnosed with right lower lobe pneumonia, new onset atrial fibrillation, and congestive heart failure. Antibiotics are administered to treat the pneumonia. Because of the history of the unexplained sinus tachycardia during her recent physician visit and the undetectable TSH, the patient is suspected to have undiagnosed thyrotoxicosis. The Burch-Wartofsky score is calculated, yielding a value of 105 out of a possible 140. Thyroid storm is highly likely. Appropriate laboratory studies were ordered, treatment for thyroid storm initiated and the patient admitted to the ICU. After a 6-day hospital stay, the patient is discharged home to her family.
Pearls and Pitfalls
- Suspect thyroid storm in any patient with a history of thyroid disease (esp. thyrotoxicosis) and a hypermetabolic state.
- The diagnosis of thyroid storm is a clinical diagnosis.
- Always look for the trigger (ex. infection, myocardial infarction, etc.)
- Initiate thiourea treatment before starting iodine therapy.
- These patients are critically ill and have a significant mortality rate, even with appropriate therapy.
References
- Burch HB, Wartofsky L: Life-threatening thyrotoxicosis. Thyroid storm. Endocrinol Metab Clin N Am 1993;22(2):263-77.
- Devereaux D, Tewelde SZ: Hyperthyroidism and Thyrotoxicosis. Emerg Med Clin N Am 2014;32:277-92.
- Galindo RJ, Hurtado CR, Pasquel FJ, et al: National Trends in Incidence, Mortality, and Clinical Outcomes of Patients Hospitalized for Thyrotoxicosis With and Without Thyroid Storm in the United States, 2004-2013. Thyroid 2018;10(10):1-8.
- Mills L, Lim S: Identifying and treating thyroid storm and myxedema coma in the Emergency Department. Emerg Med Pract 2009;11(8).
- Nayak B, Burman K: Thyrotoxicosis and thyroid storm. Endocrinol Metab Clin N Am 2006;35:663-86.
- Ross DS, Burch HB, Cooper DS, et al.: 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid 2016;26(10):13431421.
- Wartofsky L, Kubo-Gwiezdzinska J. 2019. Thyroid Storm (Thyrotoxic Crisis). In M Luster, LH Duntas, L Wartofsky (Eds), The Thyroid and Its Diseases: A Comprehensive Guide for the Clinician. Pages 357-366. SpringerLINK ebook. Accessed 3\20\2019.