Cardiac Arrest
Case Study
“Physician to the Resuscitation Bay Stat!” Upon arriving to the bay, you find EMS performing CPR on a patient. EMS gives the report that they were called out for a 69-year-old female complaining of general illness and dizziness. When they arrived, the patient was in no distress and was stable en route. Just prior to pulling into the ED, she became unresponsive, pulseless, and apneic.
Objectives:
Upon completion of this self-study module, you should be able to:
- Describe the BLS Primary survey
- Describe the ACLS Secondary survey
- List indications for defibrillation
- List most frequent causes of Pulseless Electrical Activity
- Interpret cardiac rhythm strips
- Explain the appropriate diagnostic tests for cardiac arrest victims
Introduction
Emergency Medicine physicians must be adept at dealing with life threatening emergencies. Cardiac arrest claims over 350,000 lives a year and the majority of these events occur outside the hospital. Early initiation of cardiopulmonary resuscitation (CPR) and advanced cardiopulmonary life support (ACLS) has been shown to improve the mortality following cardiac arrest.
As you walk into the resuscitation bay, what initial steps should be taken to evaluate and manage this cardiac arrest victim?
- Perform BLS primary survey
- Obtain finger stick blood sugar
- Perform ACLS secondary survey
BLS Primary Survey
This basic approach to life support stresses early CPR and early defibrillation. The goal is to support or restore effective oxygenation, ventilation, and circulation until return of spontaneous circulation or until ACLS interventions can be initiated. These actions have been shown to significantly improve the chance of survival and neurologic outcome. As each step is assessed the appropriate critical action should be performed before proceeding to the next assessment step. Remember assess, then perform the appropriate action.
The BLS approach to cardiac arrest can be best remembered by using the acronym ABCD: Airway, Breathing, Circulation, and Defibrillation.
Infants and children generally go into cardiac arrest due primarily to airway issues. Adults go into cardiac arrest typically due to cardiac issues, therefore BLS in adults recommends checking for circulation and potential for defibrillation prior to evaluating the airway and breathing.
- Circulation: Check either a carotid or femoral pulse for at least 5 seconds, but not longer than 10 seconds. If no pulse is present, chest compressions should be initiated. Chest compressions should be performed at a rate of 100-120 beats per minute in adults, with a depth of 40 to 50mm or about 2 to 2.5 inches with minimal interruption.
- Defibrillation: If no pulse is present, the rhythm should be assessed using a manual defibrillator or an automatic external defibrillator (AED). The current recommendation is to either attach a defibrillator as soon as possible, or after two minutes of chest compressions. If the AED recommends defibrillation, or if your interpretation of the manual defibrillator is to defibrillate, then immediately after the shock is delivered chest compressions are to resume. Minimize any interruptions in chest compressions as doing so will rapidly decreased blood flow to the brain and heart, and subsequently increase the likelihood of an unsuccessful resuscitation attempt.
- Airway: Is the airway open? The airway should be opened using head tilt-chin lift or if trauma is suspected jaw thrust. If trauma is suspected, cervical immobilization must be maintained.
- Breathing: Look, listen, and feel for adequate breathing. Initiate rescue breathing with bag-valve-mask (BVM) ventilation if the patient is not adequately breathing. If it is difficult to compress air from the bag into the airway, reposition the head or perform a jaw thrust if there is suspected trauma and consider using visualization and McGill forceps to remove any obstruction. BVM ventilation can be performed using a one or two-person technique. Two breaths via BVM should be performed after 30 compressions in a non-intubated patient, while an intubated patient should receive continuous compressions while ventilations are given 8-10 times per minute.
- One Person Bag-Valve-Mask Technique: The single-handed technique is more difficult to perform especially for people with smaller hands or less experience. A tight mask seal must be maintained to prevent loss of air and can be very difficult in patients with craniofacial abnormalities or facial hair. The one-handed technique uses the thumb and index finger in a C configuration to grasp the body of the mask to form a seal while the third and fourth fingers grasp the ridge of the mandible. The fifth finger lifts at the angle of the mandible. The other hand compresses the bag. Dentures may be left in place while bagging to ensure a better seal with the mask and to prevent airway occlusion, but should be removed prior to intubation. (Please see the SAEM Breathing chapter for example)
- Two Person Bag-Valve-Mask Ventilation: The two-handed rescue technique should be employed whenever possible to improve adequacy of ventilation. One person uses both hands to apply downward pressure on the mask onto the face while simultaneously lifting the ramus of the mandible from a position above the head. The other person uses both hands to squeeze the bag. (Please see the SAEM Breathing chapter for example)
Regardless of the technique employed, adequacy of ventilation can be assessed by inspecting the chest for equal rise and fall and auscultating the chest for adequate aeration. Epigastric sounds and abdominal distention suggest gastric insufflations and poor ventilation.
ACLS Secondary Survey
The ACLS secondary survey involves more advanced, invasive techniques. It is critical to consider the differential diagnoses to appropriately identify and treat the underlying cause of cardiac arrest.
- Airway: The airway of the unconscious patient should remain patent by use of the head tilt-chin lift, jaw thrust, oropharyngeal airway, or nasopharyngeal airway. Because of the difficulty of establishing endotracheal intubation during active CPR, a supraglottic airway device, such as an IGel or King LTD is adequate. Endotracheal intubation is the most effective and definitive method of providing adequate ventilation and oxygenation. Endotracheal intubation is currently not recommended to be placed if it causes any delay in the delivery of resuscitation if adequate ventilation can be otherwise accomplished.
- Breathing: The adequacy of oxygenation and ventilation should be confirmed by assessing the rise and fall of the chest, auscultation of equal breath sounds, absence of breath sounds over the epigastrium, and monitoring end-tidal CO2 using capnometry or capnography. False readings may result from prolonged cardiac arrest and ingestion of carbonated beverages. The endotracheal tube should be secured and a chest radiograph obtained to ensure correct position relative to the carina. Remember that a chest x-ray does not ensure endotracheal intubation. Pulse oximetry and waveform capnography should always be monitored.
- Circulation: Intravenous (IV) or intraosseous (IO) access should be obtained and the patient should be placed on a cardiac monitor to assess the patient’s cardiac rhythm and appropriate drugs should be given based on ACLS guidelines. All IV medications and blood may also be administered via intraosseous access.
Differential Diagnosis for Cardiac Arrest
Consider, identify, and treat potential reversible causes, commonly referred to as the “H’s and T’s”:
- Hypovolemia
- Hypoxia
- Acidosis (H+)
- Hypothermia
- Electrolyte abnormality (Hyper/hypo K+)
- Cardiac Tamponade
- Tension pneumothorax
- Toxic Overdose
- Thrombus/PE
- Thrombus/AMI
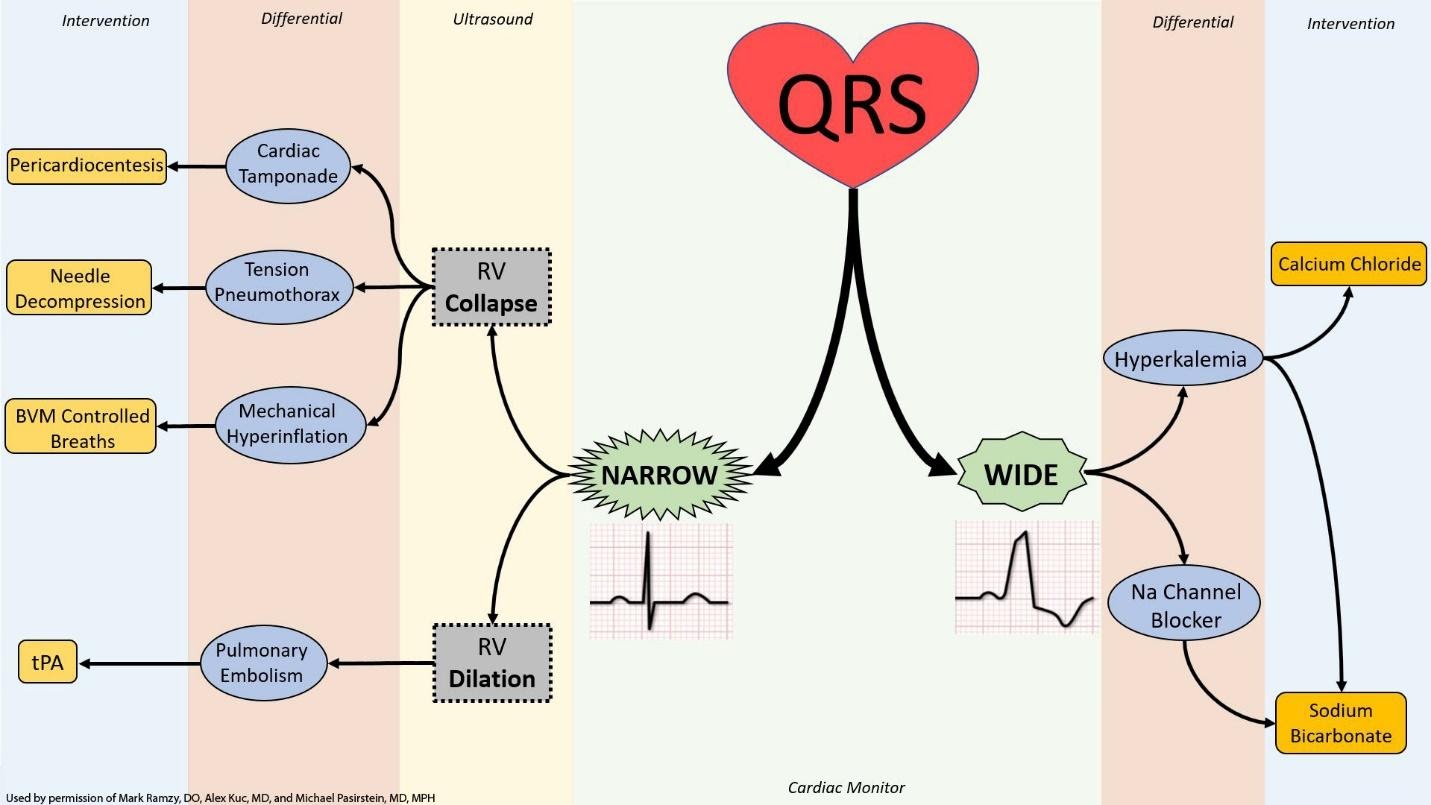
While there are recommendations to use the above pneumonic of recalling the H’s and T’s, there are alternative methods to approach the differential diagnosis of a patient in cardiac arrest. One example is to use the rhythm strip to determine if the QRS complex is wide or narrow.
- Obtain history and events surrounding arrest
- Perform physical exam that may give clues to cause of arrest
- Perform appropriate diagnostic studies. Point of Care ultrasound may be used to evaluate cardiac activity and aid in the differential diagnosis and treatment modalities.
Treatment
You perform the BLS primary survey. No carotid pulse can be palpated within 10 seconds. Chest compressions commence at a rate of 100/minute with full recoil and adequate depth. As soon as possible, the patient is placed on a monitor and the following rhythm strip is observed:

https://commons.wikimedia.org/wiki/File:Lead_II_rhythm_ventricular_tachycardia_Vtach_VT.JPG (public domain)
The above rhythm demonstrates pulseless ventricular tachycardia. Almost all episodes of sudden cardiac death initiate from a ventricular tachydysrhythmia. Successful resuscitation is dependent on rapid defibrillation. Improved survival is related to witnessed arrest with initiation of early bystander CPR, initial shockable rhythm, and rapid defibrillation and initiation of ACLS by a trained professional within 10 minutes of onset.
Once pulseless ventricular tachycardia (VT) or ventricular fibrillation (VF) is identified, the patient should be immediately defibrillated using the manufacturer’s recommended energy amount, which is typically 200 Joules (J) on a biphasic defibrillator. ACLS recommends chest compressions should only be interrupted, for less than 10 seconds, for ventilation (if an advanced airway is not in place), pulse check/rhythm check, and shock delivery.
You defibrillate your patient once with a biphasic defibrillator at 200J. How should you proceed?
CPR should be resumed immediately after the shock, and the next pulse/rhythm check should occur after 2 minutes (or 5 cycles) of CPR. In patients without an advanced airway, each cycle consists of 30 compressions and 2 ventilations. After 2 minutes of CPR, the pulse and rhythm should be rechecked, but the interruption in CPR should not exceed 10 seconds.
You cannot palpate a pulse within 5 seconds and you see the following rhythm strip. What should you do next?

https://commons.wikimedia.org/wiki/File:V_f.png (public domain)
The rhythm strip demonstrates VF. The patient should be immediately defibrillated. CPR should be again resumed immediately after the shock is delivered and continue for 2 minutes. Once IV/IO access has been established, epinephrine 1mg should be administered every 3 to 5 minutes. You should continue CPR for 2 minutes until the pulse and rhythm is checked again. If the patient remains in VF, you should consider giving antiarrhythmics including amiodarone or lidocaine. Magnesium may be given for torsades de pointes.
Despite the above interventions, the patient remains pulseless. The next rhythm check reveals the following rhythm:

What is this rhythm and how should you proceed? https://commons.wikimedia.org/wiki/File:Normal_Sinus_Rhythm_Unlabeled.jpg (public domain)
Without a pulse, this represents PEA (pulseless electrical activity). The ability to resuscitate the patient is dependent on effective CPR and the ability to identify any reversible etiologies of the arrest. Epinephrine 1mg should be administered every 3-5 minutes. No vasopressor medications have been shown to improve the survival rate to discharge but are nonetheless still recommended in ACLS for PEA and asystole. Patients with PEA and asystole have poor outcomes, but the identification of the underlying etiology is extremely important and the common causes should be reviewed, treated, or excluded during the resuscitation.
Despite 30 minutes of resuscitation efforts, your patient remains pulseless and the following rhythm is obtained during your final pulse check:

This rhythm strip demonstrates asystole. Both asystole and PEA are treated using the same ACLS algorithm. Routine transcutaneous pacing for asystole has not been shown to improve survival. The duration of the cardiac arrest is the most important prognostic factor for survival. Studies have shown that resuscitation efforts are unlikely to be successful after 20-25 minutes of combined BLS and ACLS. It is appropriate to consider cessation of resuscitation efforts at that time.
Post-Resuscitation care or Termination of Resuscitation
Termination of Resuscitation
There is no standard indication for termination of resuscitation (TOR). Common factors included in the decision to terminate are:
- Failure to obtain return of spontaneous circulation
- 20-25 minutes of an unwitnessed cardiac arrest
- 30 minutes for witnessed arrest
- Rhythm is asystole
- Persistent end-tidal CO2 <10 mmHg Obtain a 12-lead
Return of Spontaneous Circulation
If the resuscitation is successful, and you get return of spontaneous circulation (ROSC), then there are some immediate actions to perform:
- Obtain a set of vital signs
This will help determine any additional interventions, such as the management of persistent hypotension, or any tachy or brady dysrhythmia, and correct any hypoxia.
- Consider a definitive airway with an endotracheal tube with waveform capnography, if not already performed
- Obtain a 12-lead EKG: More than one-half of arrests in the US are cardiac in origin and the EKG can offer evidence of cardiac ischemia, various toxin exposure, or hyperkalemia.
- Coronary Reperfusion: Discuss with interventional cardiology team to determine if the patient is a candidate for immediate or urgent percutaneous coronary intervention (PCI)
- ABG: can show the acid-base and oxygenation status of the patient, but typically obtained after 15-20 minutes after ROSC to allow for some normalization of acid-base derangement from the arrest itself
- Serum electrolytes
- Chest X-ray
- Perform a thorough exam
If the patient does not follow commands, consider Targeted Temperature Management (TTM), or cooling of the patient. The survival rate of out of hospital cardiac arrest remains very poor despite years of prehospital advanced life support. Of those patients who have ROSC after cardiac arrest, about 10% will survive until hospital discharge. A large proportion of these victims will suffer anoxic brain injuries. Initiation of mild hypothermia, known as targeted temperature management, or TTM (cooling to 32-360 C) may potentially lead to improved functional recovery at hospital discharge. Each facility that performs TTM will have their own inclusion and exclusion criteria, and initiation should be coordinated with the accepting intensive unit team.
Pearls and Pitfalls
Managing a cardiac arrest can be mentally and emotionally taxing. Being methodical with each resuscitation will help mitigate the nuances of each individual patient.
Talk to family or bystanders, who may offer insight into the events that led up to the arrest, such as recent history of long trip or known to abuse drugs.
The physical exam during the resuscitation can help suggest possible causes for the arrest. For example, if dialysis access is noted, then perhaps the patient is hyperkalemic.
Minimize interruptions in CPR. Absence of chest compressions for more than 10 seconds is associated with decreased chance of ROSC.
Closed loop communication helps facilitate a smooth resuscitation and recognizes the importance of all members of the team.
Inclusion of family members to witness the resuscitation is unique for each patient, but it can aid in the bereavement process for the family as well as the healthcare team.
Additional research is being conducted on the utility of the addition of esmolol, ECMO, and/or dual-sequence defibrillation for the treatment of refractory ventricular fibrillation.
Case Study Resolution
CPR was initiated and high quality chest compressions were performed. The patient was endotracheally intubated and ACLS protocols were initiated. After 2 rounds of ACLS, ROSC was obtained, and vital signs were obtained. A 12-lead EKG demonstrated significant ST segment changes. The interventional cardiology team was notified, and the patient was taken for emergent PCI. The cardiology team agreed to begin cooling measures during PCI. The patient was admitted to the intensive care until following PCI.
References
1.Cheskes S, Schmicker RH, Verbeek PR, et al. The impact of peri-shock pause on survival from out-of-hospital shockable cardiac arrest during the Resuscitation Outcomes Consortium PRIMED trial. Resuscitation. 2013;85(3):336–342. doi:10.1016/j.resuscitation.2013.10.014
2.Littmann et al. A Simplified And Structured Teaching Tool for the Evaluation and Management of Pulseless Electrical Activity. Med Princ Pract 2014; 23: 1 – 6. PMID: 23949188
3. Panchal AR, Berg KM, Kudenchuk PJ, Del Rios M, Hirsch KG, Link MS, Kurz MC, Chan PS, Cabañas JG, Morley PT, Hazinski MF, Donnino MW. 2018 American Heart Association focused update on advanced cardiovascular life support use of antiarrhythmic drugs during and immediately after cardiac arrest: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2018;138:e740–e749. DOI: 10.1161/CIR.0000000000000613.https://cpr.heart.org/AHAECC/CPRAndECC/ResuscitationScience/UCM_477263_AHA-Cardiac-Arrest-Statistics.jsp%5BR=301,L,NC%5D
Author 2019: Michael Pasirstein, MD, MPH, Drexel University College of Medicine, Philadelphia, PA
Author 2008: Luan Lawson, MD, Brody School of Medicine at East Carolina University, Greenville, North Carolina
Editor: Sheena Punnapuzha MD, MPH, The Brooklyn Hospital Center, Brooklyn, NY
Last Updated: September, 2019
