Pelvic Pain and Vaginal Bleeding
Author Credentials
Authors: Elena A. Kossyreva, MD, and Jamie Aranda, MD, Department of Emergency Medicine, Medical College of Wisconsin
Editor: Matthew Tews, DO, MS, Professor of Emergency Medicine and Hospitalist Services, Medical College of Georgia
Objectives
- Obtain a focused gynecologic history and perform a pelvic examination
- Construct a broad differential diagnosis for pelvic pain and vaginal bleeding
- Discuss management of the unstable patient with pelvic pain and vaginal bleeding
- Discuss the management of the most common and emergent etiologies of pelvic pain and vaginal bleeding.
Cases
Case #1
A 23-year-old G2P1011 presents to the emergency departmentcomplaining of lower abdominal pain and vaginal discharge for the past week. She also noticed some spotting over the last 2 weeks. Her BP is 128/76, HR 86, RR 16, Temp 98.8F. The patient appears well and in no distress.
Case #2
A 28-year-old G3P0121 presents with vaginal bleeding and abdominalpain that started a week ago. This morning, the pain got suddenly worse and the patient feels lightheaded. She also mentions that her right shoulder hurts. When asked for a urine sample, the patient states that she and her partner use condoms and insists that there is no way that she could be pregnant. Her BP is 86/48, HR 124, RR 22, SpO2 98%, Temp is 99.6F.
Introduction
Acute pelvic pain is defined as pelvic pain of less than 6 months duration. It may be of gynecologic, obstetric, gastrointestinal, urogenital or even vascular origin (Table 1).
Table 1: Causes of Acute Pelvic Pain
| Gynecologic | Obstetric | Gastrointestinal | Urogenital | Vascular |
| Ruptured ovarian cyst | Round ligament pain | Appendicitis | Urinary tract infection | Deep vein thrombosis |
| Pelvic inflammatory disease | Ectopic pregnancy | Irritable bowel syndrome | Ureteral colic | Pseudoaneurysm |
| Tubo-ovarian abscess | Abortion | Inflammatory bowel disease | ||
| Adnexal torsion | Placental abruption | Bowel obstruction | ||
| Dysmenorrhea | Diverticulitis | |||
| Mittelschmerz | Hernia | |||
| Endometriosis |
The differential diagnosis in vaginal bleeding is different for pregnant and non-pregnant patients. In a pregnant patient, determining whether the pregnancy is ectopic is of great importance as it is one of the leading causes of maternal morbidity and mortality in the United States. The date of the patient’s last menstrual period (LMP), the duration of the menses and the amount of bleeding should be obtained in women who present with vaginal bleeding. Normal menstrual blood loss is 20-60 ml per cycle. If blood loss exceeds 80 ml and occurs at irregular intervals, it is termed menometrorrhagia. In neonates, vaginal bleeding may be normal if it occurs within the first 10 days of life and is due to withdrawal from maternal estrogen exposure. Other potential causes of vaginal bleeding are listed in Table 2.
Table 2: Causes of Vaginal Bleeding
| Category | Diagnosis |
| Pregnancy | Ectopic |
| Anatomic | Fibroids |
| Coagulopathy | Von Willebrand Disease |
| Endocrine | Polycystic ovary syndrome |
Infectious | Sexually transmitted infection Urinary tract infection |
| Medications | Birth control pills |
Despite a broad differential diagnosis, a focused, yet thorough, history and physical examination (including gynecologic, obstetric, social history and pelvic exam) along with laboratory work-up and imaging will help determine the origin of pelvic pain and/or vaginal bleeding.
Initial Actions and Primary Survey
As with any patient in the ED, first consider airway, breathing and circulation (the ABC's) in the patient with pelvic pain and vaginal bleeding. Circulation may need to be addressed immediately if the bleeding is heavy or if they have symptoms of poor perfusion such as altered mentation, dizziness, or difficulty breathing. If circulation is inadequate to perfuse the patient’s brain, this may lead to an airway or breathing problem requiring intubation to protect the airway as well as aggressive volume resuscitation. In the hemodynamically unstable patient, placing two large-bore intravenous lines is a priority, followed by resuscitation with crystalloid fluids followed by blood products (i.e. packed red blood cells) if there has been enough blood loss.
If the source of bleeding is suspected to be a potential ectopic pregnancy, the patient's pregnancy status needs to be established as soon as possible. If positive, it is crucial to determine whether the pregnancy is intrauterine or extrauterine, as a ruptured ectopic is a surgical emergency requiring emergency laparoscopy. Identification of pregnancy location can be accomplished with bedside ultrasonography in the unstable patient. If intrauterine pregnancy cannot be identified on bedside ultrasound, OB/GYN should be consulted immediately for potential surgical management. The LMP and gestational age should be determined as they are important components of the patient’s history to help guide management.
Perform a formal pregnancy test on your pelvic pain and vaginal bleeding patients of childbearing age as soon as possible. Of note, the urine pregnancy test is 99.4% sensitive for diagnosing pregnancy at the time of a missed period. False negatives occur when the urine is diluted and when serum β-hCG level is 10-50 mIU/ml.
If the urine pregnancy test is negative and suspicion remains high, continue to pursue ectopic pregnancy as the leading diagnosis as above. If other potential causes of pelvic pain are suspected based on history and the patient’s vaginal bleeding may be a part of their menses, then further management should be determined on a case-by-case basis.
History and Physical Examination
When obtaining history from a female patient presenting with pelvic pain and/or vaginal bleeding, there are several questions that should be asked.
All women with gynecologic concerns should be asked about their gynecologic history regardless of whether they are pregnant. Questions to ask:
- Last menstrual period, frequency and amount of bleeding
- Contraception use
- If currently sexually active
- Sex and number of partners
- Dyspareunia
- History of sexually transmitted diseases and whether they were treated
- Previous pregnancies and delivery method
- Previous gynecologic procedures
If she is pregnant, establish the patient’s obstetric history by asking about prior pregnancies as well as the current one. GTPAL is a commonly used system that summarizes this data:
- G (gravida): number of pregnancies
- T (term births): number born at>37 weeks
- P (premature births): number born at<37 weeks
- A (abortions): number of abortions or miscarriages
- L (live): number of living children
For example, a woman comes in with her fifth pregnancy. She has three living children (one born at 35 weeks and two at 38 and 39 weeks). She also had a prior abortion. According to the GTPAL system, she is G-5, T-2, P-1, A-1, L-3 (this is abbreviated as G5P2113).
Once all of the pertinent information is gathered from the patient, the next step is to perform a pelvic examination. A chaperone should always be present during the pelvic exam, even when the examiner is a female provider. Prior to performing a pelvic exam, all components of the exam should be set up. Below is an example of a typical pelvic exam setup.
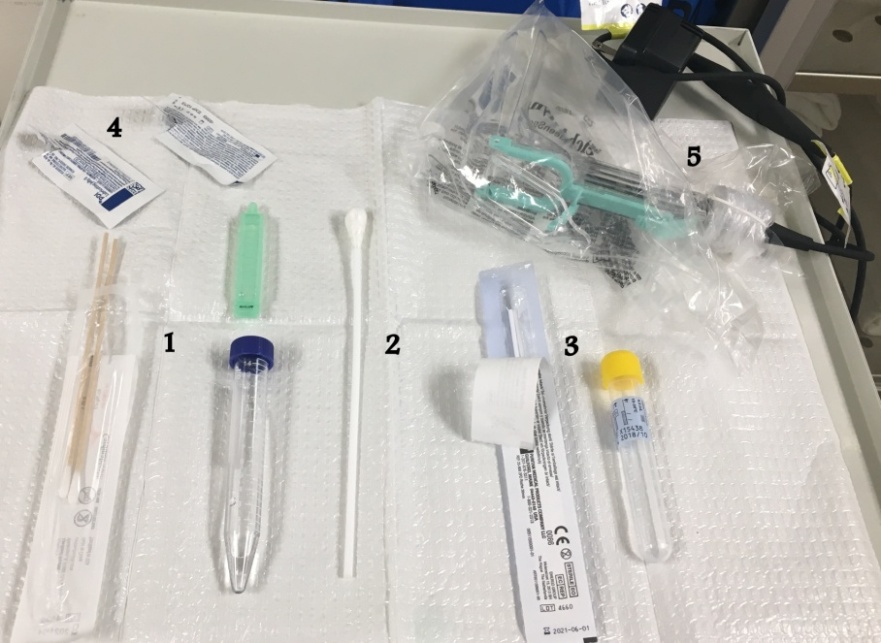
Pelvic exam setup
- Wet mount swabs, test tube and liquid.
- Large swab (typically used to clear vagina of blood/secretions in order to visualize the cervix or source of bleeding).
- Gonorrhea and chlamydia swabs and test tube.
- Lubricant jelly for speculum and bimanual exams.
- Speculum with a light source.
When performing the pelvic exam, always start by visualizing the external genitalia and anus for lesions. Carefully examine the vagina and cervix, especially in the bleeding patient, to assess for lacerations or lesions that may be causing bleeding. Look for signs of products of conception protruding from the cervix or in the vaginal canal. Collect cervical specimens and send them to the lab even if you do not initially intend on testing, as you do not want to have to repeat an invasive exam unnecessarily. Common tests performed on the specimens look for bacterial vaginosis, yeast and trichomonas (wet mount) as well as chlamydia and gonorrhea. Wet mount specimens are typically collected from the posterior fornix while either endocervical or vaginal swabs are appropriate for the gonorrhea and chlamydia Nucleic Acid Amplification Test (NAAT). The wet mount typically results while the patient is still in the ED, while chlamydia and gonorrhea take up to three days to result. If you suspect that your patient is at a high risk for these infections, you may recommend and provide empiric antibiotic treatment.
Following the speculum examination, a bimanual exam is performed to assess the adnexa, cervix and uterus. Your patient's body habitus may limit this part of gynecologic examination, particularly if they are obese. Note that the bimanual exam is contraindicated in pregnant patients with placenta previa. If you suspect the patient is pregnant and possibly in their second trimester with unknown placental location (possible previa), defer this portion of the exam to the obstetrician or until an ultrasound is complete and the location of the placenta is known.
Treatment
The treatment of common causes of pelvic pain and/or vaginal bleeding are covered in this chapter. Treatment recommendations listed should always be checked with updated management guidelines and hospital susceptibility data. Further detail on the management of ectopic pregnancy, pelvic inflammatory disease/tubo-ovarian abscess and ovarian torsion can be found in the M4 Curriculum.
Infectious Etiologies
Antibiotic regimens for infectious causes of pelvic pain are listed in Table 3.
Cervicitis due to Gonorrhea or Chlamydia
Consider both gonorrhea and chlamydia in patients with pelvic complaints and high risk sexual behavior. With gonorrheal infection, symptoms may not be limited to the urogenital tract. Pharyngeal, rectal and ocular infections are also possible. In women, urogenital infections (cervicitis, urethritis) present with abnormal vaginal discharge, intermenstrual bleeding, dysuria, dyspareunia or lower abdominal pain. There may be mucopurulent discharge from the cervical os in gonococcal cervicitis. When treating empirically in the ED, provide coverage for both organisms.
Pearls
- Adding azithromycin not only covers chlamydial infection, it also provides dual coverage for gonorrhea given its resistance to antimicrobials;
- Untreated infection in women may lead to PID, ectopic pregnancy and infertility;
- Remember to recommend treatment to their partner.
Trichomoniasis
Acute infection presents with purulent, foul, thin discharge with burning, itching lower abdominal pain and dyspareunia. Patients may also have postcoital bleeding. Vulva and vaginal mucosa appear erythematous. Greenish, frothy, malodorous discharge is sometimes present. "Strawberry cervix" is rarely present. Motile trichomonads are seen on wet mount and diagnosis can also be made by a positive culture, NAAT or rapid antigen probe test. Trichomoniasis is treated with 5-nitroimidazole drugs only (metronidazole or tinidazole):
Pearls
- Recommend treatment to partners and recommend no sexual intercourse for 7-10 days;
- Commonly coexists with bacterial vaginosis (same treatment);
- Also test for chlamydia and gonorrhea when trichomoniasis is present or suspected;
- Trichomoniasis is associated with adverse outcomes during pregnancy.
Bacterial vaginosis (BV)
Caused by rising vaginal pH (>4.5, normal range is 4.0-4.5) due to a shift in vaginal flora. About 50-75% of women are asymptomatic, but others present with thin, grayish vaginal discharge and/or odor that is described as "fishy." If your patient also complains of dysuria, burning, itching or other symptoms, consider mixed vaginitis (>1 pathogen).
Per Amsel criteria, three of the following must be present for diagnosis of BV
- Thin, grayish discharge
- Vaginal pH >4.5
- Positive "whiff test" (fishy odor when KOH is added to a sample of discharge)
- Clue cells on wet mount (>20%)
Pearls
- Instruct patient to avoid alcohol while taking metronidazole as well as 1 day following completion of treatment to avoid disulfiram-like reaction (nausea, vomiting, flushing, tachycardia, shortness of breath);
- BV is technically not considered an STI, although certain sexual practices increase the risk of BV.
- BV is treated with a 7-day course of metronidazole; the metronidazole 2 gm PO single dose regimen is no longer recommended due to lower efficacy
Yeast (vulvo-vaginal candidiasis)
Patients present with vaginitis symptoms (pruritis, burning, soreness, dysuria or dyspareunia). Higher risk patients are those with diabetes, antibiotic use, oral contraceptive use, pregnancy and immunosuppression. Candida is seen on wet mount. Vaginal pH is typically normal. Treatment is targeted at symptom relief.
Pearls
- Yeast infection is not considered an STI;
- Self-diagnosis is often inaccurate.
- Treatment with Fluconazole may be extended in complicated candidiasis
Pelvic Inflammatory Disease (PID)
Patients present with vaginal discharge, acute bilateral lower abdominal pain, dyspareunia and post-coital bleeding. On exam, there is cervical motion and adnexal tenderness as well as mucopurulent cervical discharge. WBCs are seen on wet mount. Some also have leukocytosis on CBC. Treatment includes PO/IM route for mild-to-moderate PID.
Pearls
- Add Metronidazole to the treatment regimen if unsure whether extended anaerobic coverage is needed as 3rd generation cephalosporins provide limited anaerobic coverage.
Urinary Tract Infection (UTI)
Patients may present with dysuria, urinary urgency, frequency, pelvic pain and hematuria. Urinalysis and urine culture should be obtained.
Pearls
- For discomfort, recommend OTC phenazopyridine (Azo OTC) PO TID as needed;
- Asymptomatic bacteriuria in pregnant women should always be treated as it is associated with adverse pregnancy outcomes.
Table 3: Common Antibiotic Treatment for Infectious Etiologies of Pelvic Pain
| Etiology | Treatment |
| Cervicitis | Ceftriaxone 250mg IM single dose PLUS Azithromycin 1 gram PO single dose |
| Trichomoniasis | Metronidazole 2 gm PO single dose OR Metronidazole 500 mg PO BID x 7 d |
| Bacterial Vaginosis | Metronidazole 500 mg PO BID x 7 d |
| Candidiasis | Fluconazole 150 mg PO single dose |
| Pelvic Inflammatory Disease | Ceftriaxone 250 mg IM single dose PLUS Doxycycline 100 mg PO BID x 14 d +/- Metronidazole 500 mg PO BID x 14 d |
| Urinary Tract Infection/uncomplicated cystitis | Nitrofurantoin 100 mg PO BID x 5 d OR TMP-SMX 160/800 mg PO BID x 3 d (non-pregnant) |
Obstetric and Gynecologic Etiologies
Ovarian torsion
Patients typically present with acute onset pelvic pain, nausea/vomiting, fever and abnormal vaginal bleeding. An adnexal mass may be palpated on examination. Labs may show leukocytosis. If ovarian torsion is suspected, order a pelvic ultrasound and promptly consult OB/GYN. Do not delay consultation if suspicion is high as definitive diagnosis is made in the OR; ultrasonography cannot rule out ovarian torsion. Obtain a pregnancy test to exclude an ectopic pregnancy. Also consider tubo-ovarian abscess and appendicitis in the differential. Definitive treatment is surgical.
Ectopic pregnancy
Patients present with amenorrhea, irregular spotting, pelvic pain, missed period, history of PID, prior ectopic pregnancy. Pain becomes acutely worse with a ruptured ectopic and may lead to syncope. Patients may complain of shoulder pain due to blood irritating the diaphragm. On exam, evaluate for abdominal or adnexal tenderness. Sometimes an adnexal mass can be palpated. Obtain beta hCG level and pelvic ultrasound to locate the fetus.
A ruptured ectopic pregnancy is a surgical emergency while treatment of a simple ectopic pregnancy is either surgical (via laparoscopy) or medical (methotrexate; one-time low-dose IM injection if ectopic is < 4 cm in diameter). For patients receiving methotrexate, a beta hCG level is repeated and if not decreasing, repeat dosing of methotrexate is required, however this is typically managed by OB/GYN in outpatient follow up.
Pearls
- Consider this diagnosis in a hemodynamically unstable female with pelvic pain and spotting;
- Note that when the hCG level is 1500-2000 mIU/mL, you should be able to see an intrauterine gestational sac on transvaginal ultrasound. Pregnancy of undetermined location on US with a beta hCG in this range is concerning for ectopic pregnancy.
Abortion
Spontaneous abortion is defined as loss of pregnancy before 20 weeks’ gestation or loss of a fetus weighing < 500 gm. About 75% of these occur before 8 weeks. The most common presenting complaint is bleeding with or without associated pelvic pain. These are definitions of the types of abortions:
Threatened: VB in the first 20 weeks, closed cervical os, no passage of tissue
Inevitable: dilated cervix
Incomplete: partial passage of tissue
Complete: passage of all fetal tissue before 20 weeks
Missed: fetal death < 20 weeks without passage of tissue for 4 weeks after fetal death
Septic: evidence of infection during any stage of abortion (fever, pelvic pain, drainage)
Evaluation for an abortion includes a pelvic exam, labs (including hCG, Rh factor and UA) and ultrasound.
Treatment
- Rh-negative women should receive anti-Rho (D) immunoglobulin (50-300 ug).
- Consider dilation and curettage or medical treatment (e.g., misoprostol) in consultation with obstetrician.
Septic abortion requires antibiotics:
- Ampicillin/sulbactam 3 gm IV OR
- Clindamycin 600 mg IV PLUS
- Gentamicin 1-2 mg/kg IV
Pearl
- All recovered products of conception (POC) should be sent for pathology.
Placental abruption
Placental abruption is premature separation of placenta from the uterine lining. Consider an abruption in all pregnant women near term who present with painful vaginal bleeding. Once the patient is stabilized, perform an ultrasound to evaluate for placenta previa (bimanual exam would be contraindicated if placenta previa is detected). Ultrasound is not sensitive for placental abruption, but may aid in diagnosis. Fetal monitoring is necessary to detect fetal distress from a placental disruption. Depending on the extent of the abruption, it may be self-limiting or require immediate Cesarean delivery. Manage in consultation with OB/GYN.
Pearls
- Nearly 50% of cases of placental abruption present without abdominal pain;
- Do not rely on the amount of vaginal bleeding to estimate the extent of abruption.
Mittelschmerz
Patients present with pelvic pain and spotting in the middle of their menstrual cycle. Pain is unilateral and associated with ovulation. This occurs in patients who are not taking oral contraceptive pills. Perform pelvic and bimanual exams to evaluate for other pathology and obtain a urine pregnancy test. Recommend mild analgesics (NSAIDs, acetaminophen) and reassurance.
Uterine fibroids
Post-menopausal women may present with pelvic pain and vaginal bleeding. Several firm masses may be palpable over the uterus. Recommend NSAIDs, outpatient ultrasound and gynecology referral as treatment may include hysterectomy or uterine artery embolization for stable patients with persistent bleeding.
Pearl
- Consider endometrial cancer in women > 45 years old. Outpatient endometrial biopsy should be performed in this patient population.
Case Summary
Case #1:
You obtain your patient’s gynecologic and obstetric history and she admits to having been diagnosed with chlamydia in the past but does not recall if it was treated. She has been pregnant once and had a miscarriage. She is currently sexually active with two male partners. On her pelvic exam, you notice purulent cervical discharge and cervical motion tenderness. You are concerned that your patient has pelvic inflammatory disease (PID) and collect cervical specimens for wet mount and gonorrhea/chlamydia testing. Her urine pregnancy test is negative.
You are concerned that your patient has PID and offer to treat her empirically. You recall that serious complications of PID include tubo-ovarian abscess, ectopic pregnancy and infertility.
Remember that all patients diagnosed with PID are at risk of developing a tubo-ovarian abscess even if they do not have a fever. Patients with PID who present with any of the following should receive imaging (pelvic ultrasound or CT) in order to assess for tubo-ovarian abscess: those in significant pain, acutely ill, febrile patients, adnexal mass noted on exam, no response or poor response to prior antibiotic course for PID. Those who had a negative ultrasound or CT 48 to 72 hours ago and were started on appropriate antibiotics but continue to worsen should also get repeat imaging. Based on these criteria, this patient does not require imaging at this time, but you instruct the patient to come back to ED if she develops a fever, worsening pain, vomiting or any other new symptoms and provide her with Ob/Gyn clinic referral. You also review CDC guidelines for treatment of PID and administer a single dose of 250 mg IM ceftriaxone and prescribe 100 mg doxycycline po BID x 14 days. You give her toradol for pain in the ED and recommend that she take ibuprofen for discomfort at home.
Case #2
You are concerned about this patient given her hypotension, tachycardia and lightheadedness. She is able to talk to you, her airway is patent and respiratory rate is normal. You establish two large-bore IV’s, initiate infusion of 1 liter of normal saline, place the patient on the monitor and pulse oximeter and order type and cross. Her urine pregnancy test comes back positive. The patient admits to having missed her period and her LMP was 6 weeks ago. Her β-hCG serum quantitative level is 4000 mIU/mL.
You are concerned that your pregnant patient with abdominal pain, vaginal bleeding and hemodynamic instability has a ruptured ectopic pregnancy and immediately page Ob/Gyn for an emergent evaluation.You perform a FAST exam and note a large amount of free fluid in the pelvis. Her blood pressure improves with resuscitation and the first unit of PRBCs is infusing. The patient is Rh-negative, so you administer anti-Rho (D) immunoglobulin. Your surgical colleagues take the patient to the operating room.
Pearls and Pitfalls
- As with any other ED patient, start with the ABC's
- Always obtain a pregnancy test in female patients of childbearing age who present with pelvic pain or vaginal bleeding, even if the patient insists that there is no chance of her being pregnant
- Perform thorough history and exam, which include gynecologic/obstetric history and pelvic exam with specimen collection
- Keep a broad differential and rule out the most critical causes of pelvic pain and vaginal bleeding
- Do not hesitate to involve OB/GYN early if your patient is unstable
References
- Beckmann, CRB, et al. Obstetrics and Gynecology, 7thed. Lippincott-Williams & Wilkins, 2013.
- Kaufman, MS, et al. First Aid for the Obstetrics and Gynecology Clerkship, 3rd ed. McGraw-Hill, 2010, pp. 250-52.
- Tintinalli, JE, et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7th ed. Section 11: Obstetrics and Gynecology. McGraw-Hill,2010.
- Toy et al. Case Files: Obstetrics & Gynecology, 3rd ed. McGraw-Hill Medical, 2009, pp. 5-7, 246-50.
- Wolfson, AB, et al. Harwood-Nuss’ Clinical Practice of Emergency Medicine, 5th ed. Lippincott Williams & Wilkins, 2010, pp. 659-85.
