Circulation: Tachydysrhythmias
Author Credentials
Original Authors: Nicole Lopez, MD, Erich Weidenbener, MD and Jamie Aranda, MD, Department of Emergency Medicine, Medical College of Wisconsin
Original Editor: Matthew Tews, DO, MS, Department of Emergency Medicine and Hospitalist Services, Medical College of Georgia
Section Editor: Navdeep Sekhon, MD, Baylor College of Medicine
Updated: 2023
Case Study
A 35-year-old previously healthy male is brought to the emergency department via ambulance after reporting palpitations that started suddenly approximately one hour ago. He feels slightly lightheaded, but is denying any chest pain or shortness of breath. Triage vitals are as follows:BP = 110/70, P = 180, RR = 16, T = 98.5F, O2 sat = 98% on Room Air. The nurse states “we need to do something about this heart rate, don’t we,” and she hands you the following EKG:
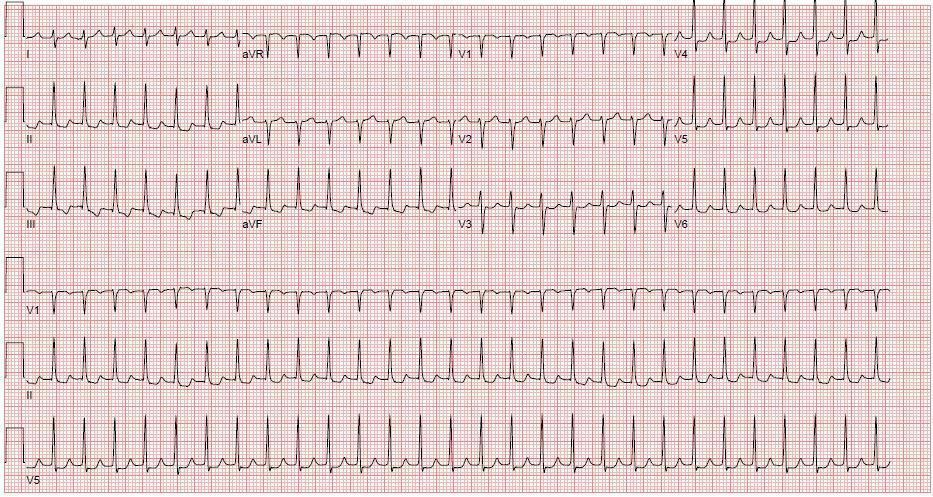
Figure 1. Paroxysmal Supraventricular Tachycardia. ECG Courtesy of Nicole Lopez, MD
You ask the nurse to obtain IV access and plan your next steps.
Objectives
By the end of this module, the student will be able to:
- Differentiate between stable and unstable tachycardias
- Understand the distinction between narrow and wide complex tachycardias
- Develop a systematic approach to the assessment and treatment of tachydysrhythmias
Introduction
A tachydysrhythmia is an abnormal rhythm with a ventricular rate greater than 100 beats/min. Given that tachydysrhythmias account for approximately 50,000 Emergency Department (ED) visits each year, the Emergency Physician (EP) must use a systematic
approach to assess patient stability and interpret the ECG in order to stabilize and treat the patient with tachydysrhythmia. Failure to rapidly recognize and treat the abnormal rhythm can result in a poor outcome for the patient.
Initial Actions and Primary Survey
With any symptomatic or unstable tachydysrhythmia, the emergency physician should always be prepared for a sudden cardiac arrest as the patient can deteriorate rapidly, thus requiring frequent reassessments. Thus, the following should be done quickly:
Obtain an ECG and IV access.
Place the patient on cardiac monitoring with pulse oximetry.
Consider placement of defibrillation pads in preparation for treatment.
Airway equipment and medications should be immediately available.
Quickly assess the stability of the patient.
If the patient is unstable, the patient should receive electrical therapy to restore sinus rhythm.
If the patient is stable, medical therapy can be attempted.
- For the stable patient, a more complete assessment including focused history, past medical history, medications, allergies, social history, family history, and physical exam may be performed
Presentation
Patients with tachydysrhythmias can present asymptomatically or with a wide-range of symptoms. The initial approach starts with an assessment of Airway, Breathing and Circulation. The emergency physician must quickly determine if the patient is stable or unstable, as this affects which treatments should be attempted.
The symptoms of a patient with tachydysrhythmia depend on the hemodynamic consequences of the abnormal rhythm. The unstable patient will have a heart rate and blood pressure that are insufficient to maintain vital organ function. Hypotension and decreased perfusion are generally more dependent on the rate rather than the source of the dysrhythmia.
Signs and symptoms of an unstable dysrhythmia include
Altered mental status
Ischemic chest pain (up to 70% of patients)
Pulmonary edema
Syncope
Hypotension
In the unstable patient, it may be necessary to obtain only an abbreviated history prior to initiating treatment.
Diagnostic Testing
After stability is assessed, the next step is an ECG. This will help determine if myocardial ischemia is present and can differentiate between tachydysrhythmias.
- Rate: The higher the rate, the more likely the patient is to be unstable. If possible, it is helpful to obtain a prior ECG for comparison.
- QRS width: After determining the rate, assess QRS width. In an adult, a QRS >120msec is considered abnormal and assumed to be ventricular in origin. Narrow complex tachycardias (QRS <120msec) are generally assumed to have a supraventricular foci.
- RR interval: Assess if the rhythm is regular or irregular by looking at the RR intervals.
- P waves: The presence or absence of P waves can differentiate between sinus tachycardia and supraventricular tachycardia (SVT), respectively. A P wave with a normal axis should be upright in lead II and negative in aVR.
The ECG algorithm organizes dysrhythmias into four categories:
Narrow complex regular:
- Sinus Tachycardia, Paroxysmal Supraventricular Tachycardia (PSVT), Atrial Flutter (Aflutter)
Narrow complex irregular:
- Multifocal Atrial Tachycardia (MAT), Atrial Fibrillation (Afib), Aflutter with variable atrioventricular (AV) conduction
Wide complex regular:
- Monomorphic Ventricular Tachycardia (VT), PSVT or Aflutter with aberrancy or bundle branch block (BBB)
Wide complex irregular:
- Polymorphic Ventricular Tachycardia aka Torsades de Pointes (TdP), Afib or Aflutter with aberrancy or BBB

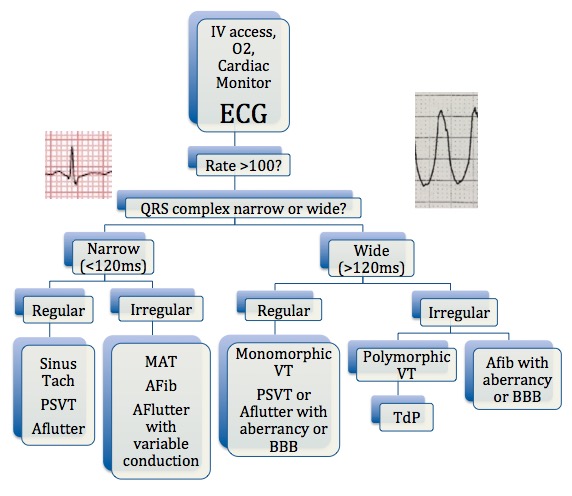 Figure 2. Diagnostic Flowchart. Created by Nicole Lopez,
MD
Figure 2. Diagnostic Flowchart. Created by Nicole Lopez,
MD
Further testing may include a telemetry strip, chest x-ray, chemistry panel, complete blood count, and cardiac enzymes. Consider infectious work-up, TSH, and toxicology screening if the clinical picture is suggestive of these underlying etiologies.
Treatment
Management of tachydysrhythmias is guided by the patient’s clinical presentation. The unstable patient may require emergent treatment prior to complete assessment. Acute management almost always relies on IV medication and/or electrical cardioversion. Electrical cardioversion or defibrillation should be used to treat any unstable tachydysrhythmia except sinus tachycardia and multifocal atrial tachycardia. A guide for medication dosing is located in a table at the end of this chapter.
Narrow Complex, Regular
The differential for this rhythm includes sinus tachycardia (ST), paroxysmal supraventricular tachycardia (PSVT), and atrial flutter (Aflutter) with a consistent AV block.
Sinus Tachycardia
This is the most common narrow complex regular tachycardia. ST is characterized by sinus P waves, normal PR interval (<200msec), 1:1 AV conduction, and an atrial rate usually 100-160 beats/min. It is typically an appropriate response to physiologic stimuli. It is important that the maximum physiologic rate that a heart can maintain can be calculated using the following equation:
Maximum heart rate= 220 - age
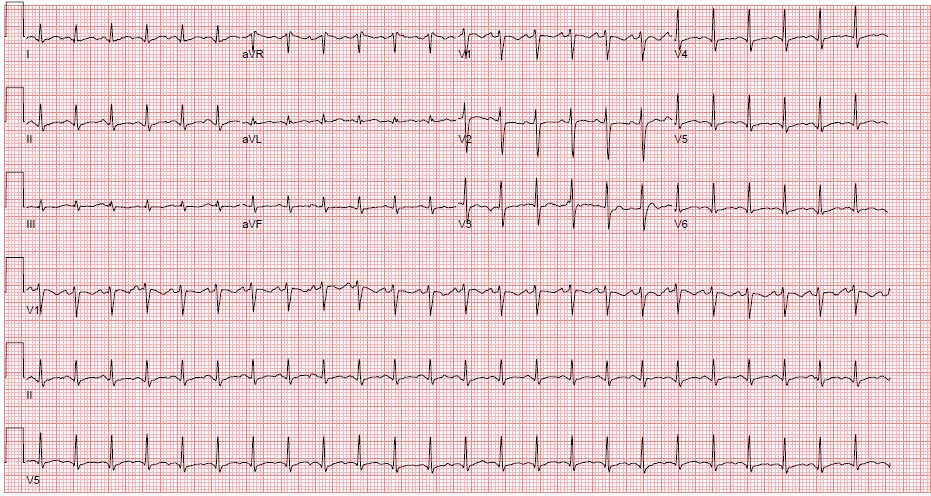
Figure 3. Sinus Tachycardia ECG Courtesy of Nicole Lopez, MD
Treatment of sinus tachycardia should address the underlying etiology rather than the rhythm itself. Common causes include: hypovolemia, sepsis, pain, alcohol withdrawal, sympathomimetic intoxication, thyroid storm, etc.
Paroxysmal supraventricular tachycardia
PSVT is characterized by a rapid and regular tachycardia of abrupt onset and termination. ECG characteristics of PSVT are
Absence of P waves
Presence of retrograde P waves (inverted and immediately adjacent to the QRS complex)
Typically a narrow QRS complex
Ventricular rate of 160-180 beats/min (though can be anywhere from 130-300 beats/min)
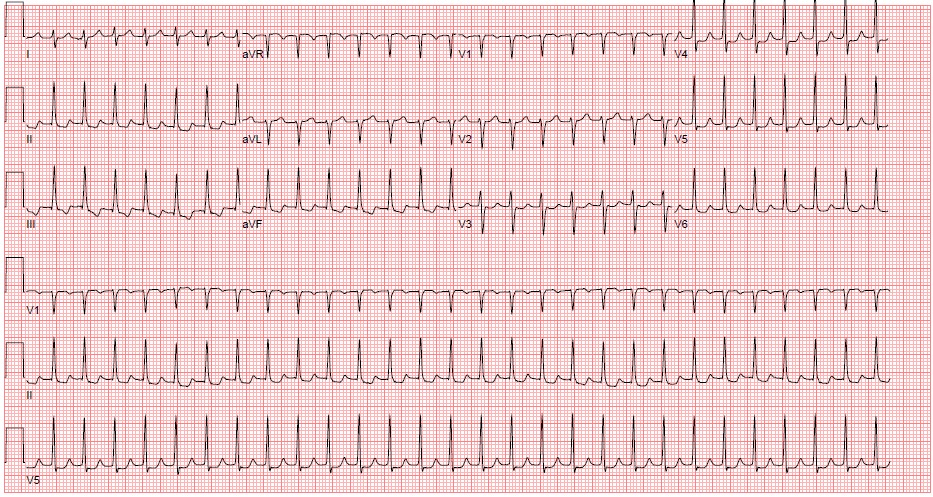
Figure 4. Paroxysmal Supraventricular Tachycardia. ECG Courtesy of Nicole Lopez, MD
If a patient has PSVT and evidence of instability, they should undergo synchronized electrical cardioversion starting at 50J (can increase if dose does not work). If the PSVT patient is stable, attempt vagal maneuvers such as:
Carotid massage
Valsalva maneuver
Ice-water immersion
If vagal maneuvers are ineffective and the patient remains stable, the next line of treatment is IV medication. Appropriate choices include Adenosine (drug of choice), the non-dihydropyridine calcium channel blockers (CCBs) Verapamil and Diltiazem, and beta blockers (BBs ). Digoxin, Amiodarone and Ibutilide are rarely used. 80-98% of patients respond to pharmacologic methods; however, if medication is ineffective, or the patient becomes unstable, proceed with electrical cardioversion.
Atrial flutter
Atrail flutter is a reentrant tachydysrhythmia that has a characteristic “saw-tooth” pattern on ECG that is best seen in leads II, III, aVF, and V1. ECG features include: identifiable P waves of a single morphology with a regular atrial rate (260-300 beats/min) and typically a narrow QRS complex. It is often associated with AV blockade, which can be regular or irregular. The most common AV block of 2:1 produces ventricular rates of about 150 beats/min. The underlying cause of atrial flutter is often any condition that contributes to atrial dilation such as heart failure, valvular disease, pulmonary hypertension, chronic pulmonary embolism, etc.
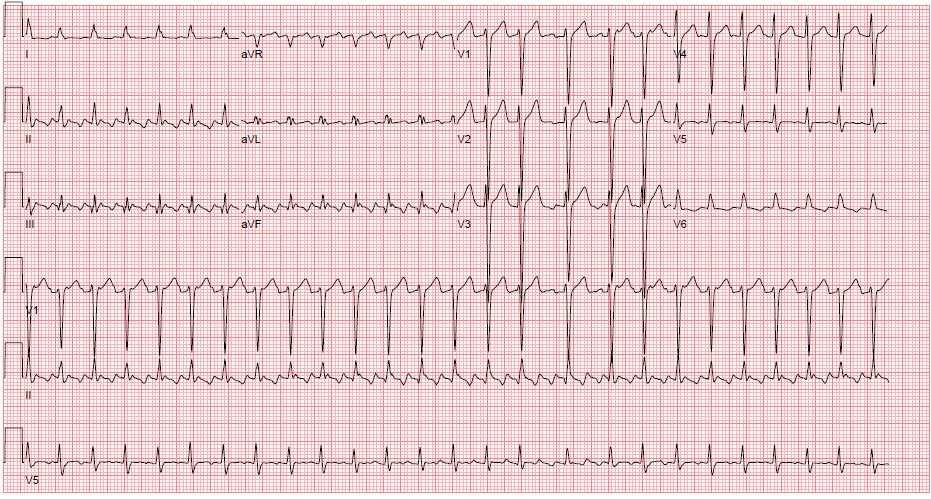
Figure 5. Atrial Flutter with 2:1 conduction ECG Courtesy of Philip Sharpless, MD
The treatment of atrial flutter depends on the patient’s clinical stability, medical comorbidities, and stroke risk. Recommendations on anti-coagulation for patients with atrial flutter are the same as those for atrial fibrillation and will be discussed in that section.
If the patient with atrial flutter is unstable, the American Heart Association recommends proceeding directly to synchronized cardioversion with 50-100J regardless of anti-coagulation status (although Aflutter is more sensitive to electricity and may convert with as little as 20-50J). Heart rates can be difficult to control in atral flutter, but cardioversion tends to be successful at lower energy levels than those required for atrial fibrillation. Pharmacologic cardioversion is generally less effective than electric cardioversion, but may be used when the patient is not able to tolerate sedation or by patient preference. Ibutilide is successful converting to sinus rhythm 60% of the time, and requires cardiac monitoring for at least four hours due to proarrhythmic effects. For rate control, options include calcium channel blockers, beta-blockers, or less often, amiodarone and digoxin.
Narrow Complex, Irregular
Multifocal Atrial Tachycardia
MAT is characterized by ECG findings of P waves of at least three different morphologies; no consistent P to P, PR, or R to R intervals; an irregularly irregular rhythm with rates usually 100-180 beats/min, an isoelectric baseline between P waves (excludes Afib and Aflutter), and a narrow QRS complex. Patients may occasionally meet all other criteria, but have a rate <100beats/min. This should be referred to as slow MAT or multifocal atrial rhythm. Clinical manifestations usually relate to the underlying illness rather than the rhythm itself.
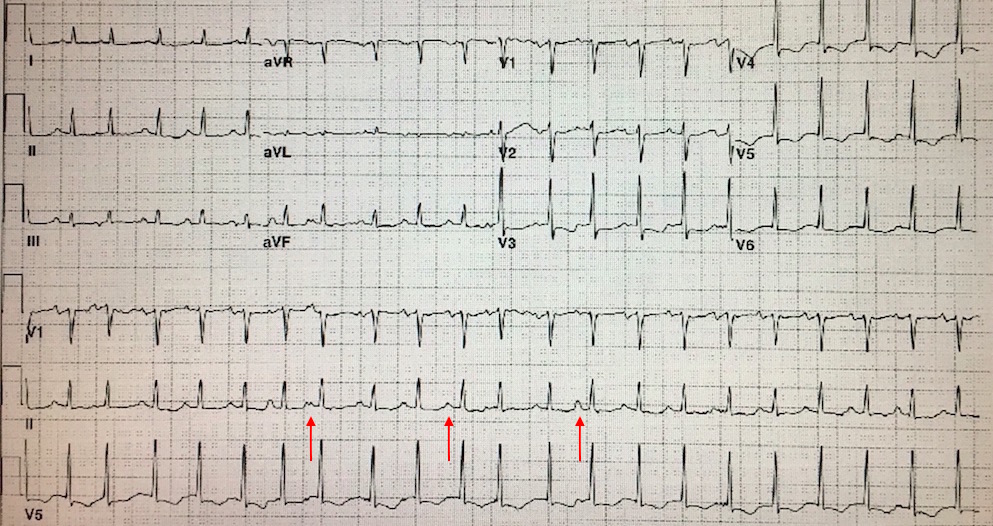
Figure 6. Multifocal Atrial Tachycardia (note arrows demonstrating differing P wave morphologies) ECG Courtesy of Philip Sharpless, MD
MAT is commonly associated with underlying conditions including pulmonary disease, pulmonary hypertension, coronary disease, valvular heart disease, hypomagnesemia, and theophylline therapy. MAT itself is rarely life threatening; however, its presence portends a poor prognosis with 40-60% of patients dying during their hospital stay due to underlying disease. Treatment is primarily directed at treating the underlying disorder. It is also important to ensure that the patient’s magnesium and potassium levels are within normal limits. If symptoms are felt to be due to the tachycardia itself, pharmacologic treatment with BBs or CCBs is an option. However, BBs should be used with caution in those with severe underlying pulmonary disease and bronchospasm. Antiarrhythmic medications and cardioversion are not indicated.
Atrial Fibrillation
A narrow complex, irregular rhythm is almost always due to atrial fibrillation (Afib) or Aflutter with a variable block. Afib is the most common dysrhythmia treated in the ED and accounts for more inpatient hospital days than any other dysrhythmia. It is due to multiple small areas of atrial myocardium continuously discharging and contracting. The atria do not depolarize and uniformly contract, but quiver resulting in decreased ventricular filling and thus decreased cardiac output. ECG characteristics include: absence of P waves with a flat or chaotic isoelectric baseline (most prominent in V1), narrow QRS complexes, and an irregularly irregular ventricular rhythm. Its hallmark is rapid, disorganized atrial activation and is often accompanied with rapid ventricular response (RVR). The atrial rate can approach up to 600 beats/min, but luckily the refractoriness of the AV node limit the ventricular rate to 120-170 beats/min.
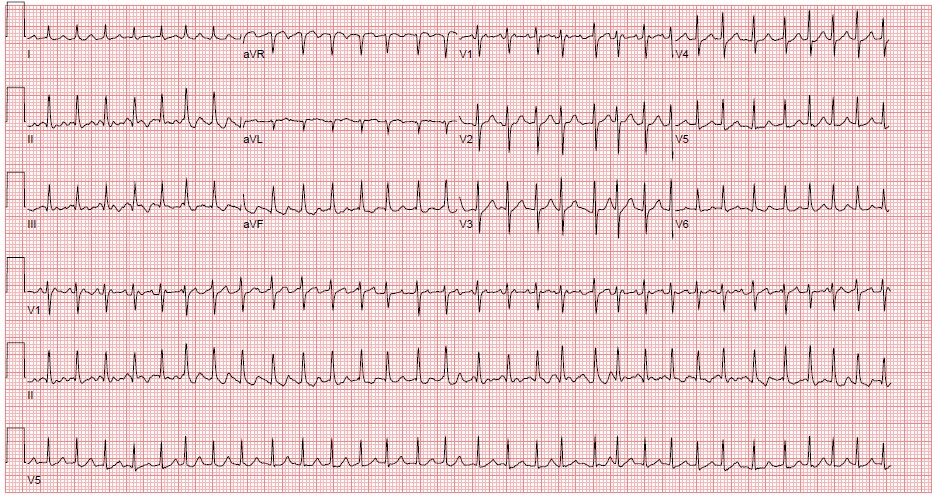
Figure 7. Atrial Fibrillation, ECG Courtesy of Nicole Lopez, MD
Afib is most commonly associated with ischemia or valvular heart disease. Other causes include congestive cardiomyopathy, myocarditis, alcohol binge (“holiday heart”) or withdrawal, pulmonary disease, pulmonary embolism, hyperthyroidism, and blunt cardiac trauma. When deciding on management options, considerations include ventricular response rate, hemodynamic status, duration of Afib, presence of underlying heart disease, and possible precipitants. Of otherwise healthy patients who present with acute-onset Afib, 70% will spontaneously convert within 48-72 hours.
For stable patients with Afib <48 hours duration, serious underlying etiology should be considered; however, 80-95% do not have an acutely critical cause and those who do will have other findings. For high-risk patients, management should include rate control and admission, but for low-risk patients, rate control followed by discharge on an oral rate control medication may be considered. Cardioversion, either chemically or electrically, has a high rate of success in these patients with an extremely low risk of stroke. Patients with uncertain duration of Afib or those at high risk of stroke should not be cardioverted in the ED unless hemodynamically unstable.
For stable patients with Afib >48 hours the primary goal is rate control. When considering which agent to use, the EP should consider the degree of symptoms, hemodynamic status, heart failure history, and potential etiology of Afib. Rate control can be achieved with CCBs, BBs, Amiodarone, or Digoxin.
Though studies have not shown any mortality benefit to a rhythm control strategy and it is logistically difficult in the ED, it may be favored in some situations. These situations include younger patient age, difficulty achieving adequate rate control, tachycardia mediated cardiomyopathy, first episode of Afib, Afib precipitated by acute illness, or patient preference. For stable patients with Afib >48 hours duration, anticoagulate for at least 3 weeks before and 4 weeks after cardioversion. IV ibutilide or procainamide are the options to restore sinus rhythm or slow ventricular rate in patients with pre-excited Afib and RVR who are not hemodynamically compromised.
In patients with Afib and Aflutter, anti-thrombotic therapy should be initiated with selection based on the patient’s risk of thromboembolism using the CHA2DS2-VASc score (Table 1) and regardless of whether the arrhythmia is paroxysmal, persistent, or permanent.
Table 1: CHA2DS2-VASc score for Atrial Fibrillation Stroke Risk
| Criteria | CHA2DS2-VASc |
| CHF | 1 |
| HTN | 1 |
| Age >= 75 | 2 |
| DM | 1 |
| Stroke, TIA, or thromboembolism | 2 |
| Vascular disease (CAD, PAD) | 1 |
| Age 65-74 | 1 |
| Gender (female) | 1 |
Low risk = CHA2DS2-VASc score of 0-1
High risk = CHA2DS2-VASc score of >=2
For patients with Afib with mechanical heart valves, Warfarin is the recommended anticoagulant with a target INR of 2.0-3.0 or 2.5-3.5 based on the type and location of the valve. For patients with non-valvular Afib and prior stroke, TIA, or CHA2DS2-VASc of ≥2, oral anticoagulation is recommended for both men and women with options including Warfarin (INR goal 2.0-3.0), Dabigatran (Pradaxa), Rivaroxaban (Xarelto), or Apixaban (Eliquis). For patients with non-valvular Afib and a CHA2DS2-VASc of 0 for men and 1 for women, it is reasonable to defer anticoagulation. Those with non-valvular Afib and a CHA2DS2-VASc of 1 for men and 2 for women are considered low-moderate risk and should be treated with either anticoagulation or antiplatelet therapy.
Patients with atrial flutter should be started on antithrombotic therapy based on the same criteria as those with Afib. If a patient with Afib of <48 hours duration, who is at low risk for thromboembolism, is successfully cardioverted, anticoagulation may not be necessary. Cardioversion is preferred in patients who are unstable, including those with decompensated heart failure, myocardial ischemia, or hypotension with the understanding that this may increase thromboembolic risk in patients with inadequate anticoagulation or uncertain duration of Afib.
For patients with increased risk for embolic complication (CHA2DS2 -VASc ≥2, mechanical heart valve, or rheumatic valvular disease) consider anticoagulation with heparin before or immediately after cardioversion. Synchronized cardioversion
is performed with 120-200J. These patients should then be anticoagulated as soon as possible for at least 4 weeks.
Wide Complex, Regular
The differential for this rhythm includes ventricular tachycardia (VT), PSVT with aberrancy, and the antidromic SVT in Wolf-Parkinson-White (WPW) Syndrome. Components of the patient’s history that make VT more likely include a history of heart disease, fusion and capture beats on ECG, and the presence of AV dissociation. Unfortunately, there is no single sign or combination of signs that can definitively identify the origin of the tachycardia. While there are several different approaches, this differentiation is beyond the scope of this chapter. Therefore, if there is any doubt, it is safest to assume that any wide-complex tachycardia is VT and treat accordingly.
Ventricular Tachycardia
VT is a macro-reentrant rhythm that is usually life threatening. It is rare in patients without underlying heart disease, with the most common causes being chronic ischemic heart disease or acute myocardial infarction. Less common etiologies include dilated or hypertrophic cardiomyopathy, valvular heart disease, inherited ion channel abnormalities, and drug toxicity. Hypoxia, alkalosis, and electrolyte abnormalities (especially hyperkalemia) exacerbate the propensity toward ventricular ectopy. ECG features of monomorphic VT are a lack of P waves associated with the QRS complex, rapid and regular rhythm; rate usually 140-180 beats/min (range can be 120-300 beats/min), and a widened QRS complex with consistent beat-to-beat morphology. Characteristics that confirm the diagnosis of VT include capture and fusion beats (Figure 8a). A capture beat (Figure 8b) is when an atrial depolarization stimulus is conducted during a time in which the ventricles are receptive. This produces a normal looking QRS in the midst of VT. A fusion beat (Figure 8a) is when atrial depolarization goes through the AV node, but then meets up with ventricular depolarization causing a mixture of a normal QRS and a PVC-like complex.
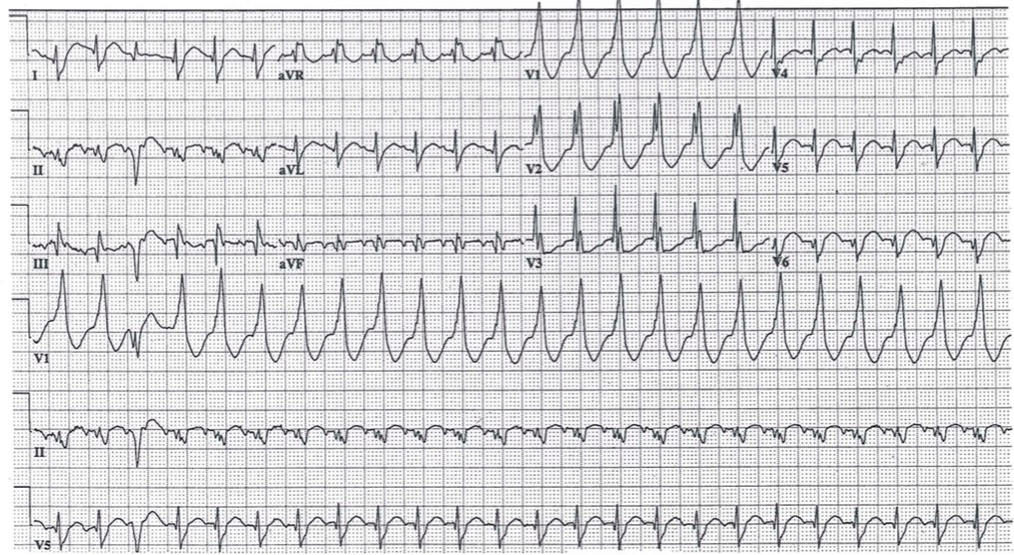
Figure 8: Ventricular Tachycardia
ECG Courtesy of Philip Sharpless
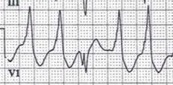
 Figure 8a: Fusion Beat
Figure 8a: Fusion Beat
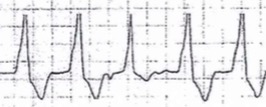
 Figure 8b: Capture Beat
Figure 8b: Capture Beat
Stable VT patients are those who are alert with no distress, have palpable pulses, a normal blood pressure, and no signs of hemodynamic compromise. Recognize that any tachydysrhythmia patient has the potential for rapid deterioration with VT being especially concerning. For the stable VT patient, treatment options most commonly consist of include Amiodarone (30% termination of arrhythmia), Procainamide (77%) or Lidocaine (27%) with the latter favored in sustained monomorphic VT associated with myocardial ischemia. Procainamide will block accessory pathway conduction which terminates preexcited tachycardias and is the agent of choice in patients with known or suspected WPW.
For the unstable VT patient with pulses, treatment is 100J cardioversion performed in the synchronized mode.
Wide Complex, Irregular
The differential for this rhythm includes Afib with a BBB or aberrancy, or polymorphic VT including torsades de pointes. If the patient has Afib with a known underlying bundle branch block, treatment is the same as if it were a narrow complex tachycardia.
Torsades de Pointes (TdP)
TdP meaning “twisting of the points” and is a form of polymorphic VT that is caused by delayed ventricular depolarization as characterized by a prolonged QT interval. ECG features of polymorphic VT are a lack of P waves associated with the QRS complex, rapid and irregular rhythm, rate usually 140-180 beats/min (range can be 120-300 beats/min), and a widened QRS complex with inconsistent beat-to-beat morphology. TdP is characterized by a progressively changing QRS complex amplitude and direction that creates a spiral pattern on the ECG.
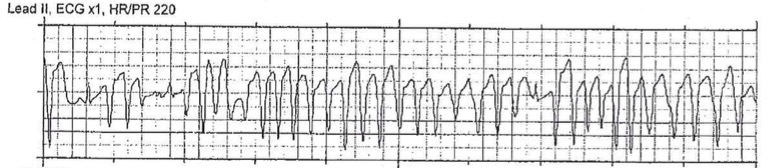
Figure 9: Torsades de Pointes. Rhythm Strip Courtesy of Dr. Philip Sharpless
The most common cause of TdP is drug-induced prolonged QT syndrome, but can also be caused by congenital prolonged QT syndrome and electrolyte derangements. Episodes can be life-threatening because they can degrade into ventricular fibrillation (Vfib). Treatment of TdP is magnesium infusion. Also important is maintaining normal serum potassium. Another option for treatment is lidocaine. Patients may have sustained episodes of TdP that lead to hemodynamic instability, in which case the treatment is unsynchronized cardioversion (i.e. defibrillation) at 200J. An alternate management option is overdrive electrical or pharmacological pacing to increase the heart rate and therefore decrease the QTc interval.
Table 2: Medication Dosing
| Medication | Dosage | Use | Notes |
| Adenosine | 6mg rapid IV push, then 12mg if SVT persists | pSVT | Follow immediately by rapid push of 20cc saline |
| Diltiazem | 0.25mg/kg IV bolus, may repeat with 0.35mg/kg IV bolus, followed by 5-15mg/hr infusion | pSVT
Afib Aflutter | Caution in advanced HF, LV systolic dysfunction, SA node dysfunction, WPW |
| Verapamil | 0.075-0.15mg/kg IV bolus, may repeat x1, followed by 0.005mg/kg/min infusion | pSVT
Afib Aflutter | Caution in advanced HF, LV systolic dysfunction, SA node dysfunction, WPW |
| Esmolol | 500mcg/kg IV bolus over 1 min, followed by 50-300mcg/kg/min infusion with repeat boluses between each dose increase PRN | pSVT
Afib Aflutter | Caution in advanced HF, SA node dysfunction, WPW |
| Metoprolol | 2.5-5.0mg IV bolus over 2 min, may repeat every 5 min up to 3 doses | pSVT
Afib Aflutter | Caution in advanced HF, SA node dysfunction, WPW |
| Propanolol | 1mg IV over 1 min, may repeat at 2 min intervals up to 2 doses | pSVT
Afib Aflutter | Caution in advanced HF, SA node dysfunction, WPW |
| Amiodarone | 150mg over 10 min (may repeat Q10min up to 2g) followed by an infusion of 1mg/min x 6hrs then 0.5mg/min x 18hrs | Afib
Aflutter VT | Less likely to cause hypotension.
Caution in pre-excitation, pregnancy |
| Digoxin | 0.25 mg IV with repeat dosing to a max of 1.5mg over 24 hours | Afib | Slow onset of action. Useful in patients with HF |
| Procainamide | 20mg/min IV followed by IV infusion at 1-4mg/min | Afib
VT | End Points: arrhythmia suppressed, hypotension, QRS increases by 50% or max dose 17mg/kg or 1000mg
Afib: Median conversion 1hr |
| Lidocaine | 1mg/kg IV over 60 seconds, may repeat 0.5mg/kg IV Q5-10 min up to 3mg/kg followed by an infusion of 1-4mg/min | VT | Use in sustained monomorphic VT associated with myocardial ischemia |
| Magnesium | 1-2g over 5-60 min, followed by 1-2mg/hr infusion | TdP | |
| Ibutilide | 0.01mg/kg up to 1mg IV over 10 min, may repeat PRN | Afib | Contraindicated in hypokalemia, prolonged QT, or HF due to risk of TdP
Median conversion 20-30mins |
ACS: Acute Coronary Syndrome; CI: contraindicated, HF: heart failure; LV: left ventricle
Table 3: Guideline for Electrical Therapy of Tachydysrhythmias
| Rhythm | Biphasic Dose |
| PSVT | 50-100J |
| Aflutter | 50-100J |
| Afib | 120-200J |
| VT with pulse | 100 |
| TdP | 200J* |
*Unsynchronized (defibrillation)
Pearls and Pitfalls
A systematic approach can be useful in the rapid assessment and treatment of the patient presenting with tachydysrhythmia
It is important to recognize the hemodynamic consequences of the rhythm
Avoid simply treating the symptoms rather than the tachydysrhythmia itself that is causing the symptoms
Consider underlying precipitants of the tachydysrhythmia such as infection, toxidromes, hypoxemia, ischemia, medication side effects, metabolic abnormalities, structural heart disease, pulmonary disease, medication non-compliance
Use caution in giving AV nodal blocking agents to the patient with Wolff-Parkinson-White with atrial fibrillation with rapid ventricular rate as this can precipitate an unstable heart rhythm
Case Study Resolution
The patient is in no distress with a reassuring blood pressure and normal mentation. His ECG shows SVT without evidence of p waves.
You diagnose the patient with SVT and attempt several vagal maneuvers including carotid massage, Valsalva, and lifting the patient’s legs into a Trendelenburg position; however, the patient’s vital signs and rhythm on the monitor
show no change.
You place a proximal IV and ask your pharmacist to draw 6mg of adenosine. This is pushed rapidly followed quickly by 20mL of saline, and the patient converts to normal sinus rhythm with a rate of 80. The patient is observed for 2 hours and has no return of his tachydysrhythmia and is discharged home with primary care physician follow up.
References
Brady, William J; Laughrey, Thomas S.; and Ghaemmaghami, Chris A. Chapter 18: Cardiac Rhythm Disturbances. In: Tintinalli JE, Kelen GD, Stapczynski JS, Ma, OJ, Cline DM, editors. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 8th ed. New York: McGraw-Hill; 2016.
Carnell, J and Singh, A. “An Evidence-Based Approach To Supraventricular Tachydysrhythmias.“ Emergency Medicine Practice. April 1, 2008. Vol 10, Num 4.
Dubin, Dale. Rapid Interpretation of EKG’s. 6th Ed. Fort Myers, Florida: Cover Publishing Company; 2000.
January et al. 2014 AHA/ACC/HRS Guideline for the Management of Patients with Atrial Fibrillation. Journal of the American College of Cardiology. Elsevier: Vol 64, No 21, December 2, 2014.
Link, Mark S. “Evaluation and Initial Treatment of Supraventricular Tachycardia.” The New England Journal of Medicine. October 11, 2012. Vol 367. Pages 1438-48.
Page, et al. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients with Supraventricular Tachycardia. Journal of the American College of Cardiology. Elsevier: Vol 67: November 13, 2016.
Schwartz, Michael; Rodman David, and Lowenstein, Steven R. “Recognition and Treatment of Multifocal Atrial Tachycardia: A Critical Review.” The Journal of Emergency Medicine. Elsevier: 1994. Vol 12, No 3, pp 353-360.
Votey, Scott R. and Silman, Eric. Chapter 85: Tachydysrhythmias. In: Wolfson AB, Cloutier RL, Hendey GW, Ling LJ, Rosen CL, Schaider JJ, editors. Harwood-Nuss’ Clinical Practice of Emergency Medicine. Philadelphia: Wolters Kluwer; 2015.
